Bradycardia (Slow Heart Rate): Symptoms, Causes, Treatment
What are the symptoms of bradycardia?
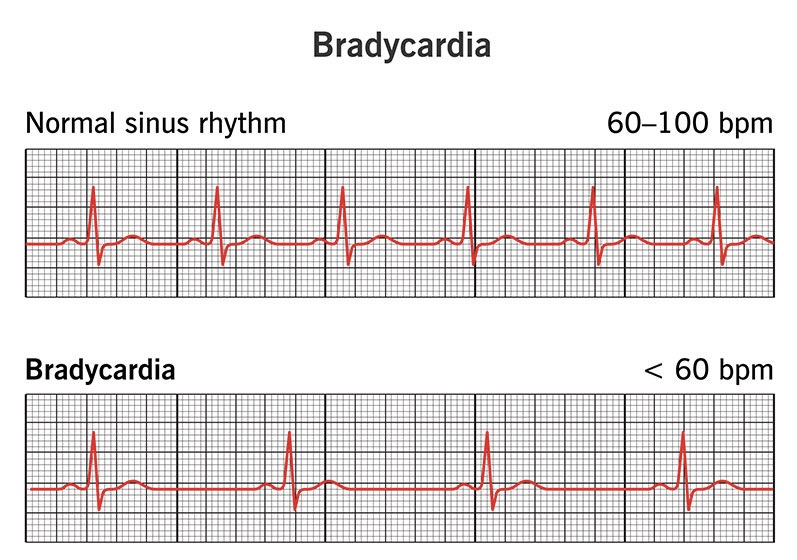
Bradycardia is a condition characterized by an abnormally slow heart rate, typically defined as a resting heart rate of less than 60 beats per minute. Some of the common symptoms associated with bradycardia include:
- Fatigue and weakness: A slow heart rate may not pump enough oxygen-rich blood to meet the body’s needs, leading to fatigue and weakness, especially during physical activity.
- Dizziness or lightheadedness: Reduced blood flow to the brain due to bradycardia can cause a feeling of dizziness, vertigo, or lightheadedness.
- Shortness of breath: Bradycardia can make it difficult for the heart to supply enough oxygenated blood to the lungs, resulting in shortness of breath or dyspnea, especially during exertion.
- Chest discomfort or palpitations: Some people with bradycardia may experience a feeling of palpitations, fluttering, or discomfort in the chest area.
- Confusion or difficulty concentrating: Inadequate blood flow to the brain can affect cognitive function and lead to confusion or difficulty concentrating.
- Fainting or near-fainting episodes (syncope): In severe cases, bradycardia can cause a temporary loss of consciousness or fainting due to insufficient blood supply to the brain.
- Easily tiring during physical activity: A slow heart rate may not be able to meet the increased demand for oxygenated blood during exercise, leading to early fatigue.
It’s important to note that bradycardia itself may not cause any symptoms in some individuals, especially if it is a longstanding condition or if the heart rate is only slightly below normal. However, the presence of symptoms may indicate an underlying health condition that requires medical attention.
What are the causes of bradycardia?
There are several potential causes of bradycardia (an abnormally slow heart rate). Some of the main causes include:
- Intrinsic heart conditions:
- Sick sinus syndrome – Malfunction of the heart’s natural pacemaker
- Heart block/conduction disorders – Impaired electrical conduction in the heart
- Electrolyte imbalances – Low levels of potassium, calcium, or magnesium
- Increased vagal tone:
- Sleep, rest, or meditation can increase vagal nerve activity slowing the heart rate
- Vasovagal response (reflex bradycardia) due to pain, stress, or environmental triggers
- An underactive thyroid gland can slow metabolic processes and heart rate
- Repeated pauses in breathing can trigger a reflex bradycardia
- Athletic conditioning:
- Athletes often have a resting bradycardia due to increased cardiovascular fitness
- Medications:
- Beta-blockers, calcium channel blockers, digoxin, certain antiarrhythmics
- Anti-seizure drugs, lithium, opioid analgesics, etc.
- Myocardial ischemia or infarction:
- Reduced blood flow or damage to the heart muscle can disrupt electrical impulses
- Increased intracranial pressure:
- Head trauma, tumors or bleeding in the brain can trigger bradycardia
- Metabolic disorders:
- Hypoglycemia, hypothermia, hypoxia can slow the heart rate
- Autonomic neuropathy:
- Nerve damage affecting autonomic regulation of heart rate
The underlying cause determines if bradycardia is pathological or a normal physiological response. Age and physical conditioning also influence what qualifies as an abnormally slow rate.
What is the treatment for bradycardia?
The treatment for bradycardia (abnormally slow heart rate) depends on the underlying cause, the severity of symptoms, and whether it is a temporary or chronic condition. Some common treatment approaches include:
Medications:
- Atropine – Short-acting drug that can temporarily increase heart rate
- Isoproterenol or dopamine – Intravenous medications to stimulate heart rate
- Discontinuing bradycardia-causing drugs if possible
Pacemaker:
- Implantation of a permanent pacemaker device is recommended for severe, chronic bradycardia not responding to other treatments
- The pacemaker electrically stimulates the heart to maintain an adequate rate
Treating underlying conditions:
- For bradycardia caused by hypothyroidism, thyroid hormone replacement
- Managing electrolyte imbalances or acid-base disorders
- Treating sleep apnea or increased intracranial pressure
Procedures:
- Transcatheter or surgical ablation to disrupt abnormal electrical pathways
- Implanting a biventricular pacemaker for certain conduction disorders
Lifestyle changes:
- For athletes with high vagal tone, reducing extreme endurance training
- Avoiding bradycardia-triggering situations like severe emotional stress
- Avoiding dehydration and avoiding hypothermia
No treatment:
- For asymptomatic cases with no underlying risk, just regular monitoring
The goal is to maintain an adequate heart rate, prevent complications like heart failure, and address any underlying conditions. Emergency treatments are needed for symptomatic bradycardia causing low blood pressure, chest pain or fainting.
Pacemaker therapy is the principal treatment for persistent, symptomatic bradycardias that medications cannot correct. Close follow-up is needed to monitor heart rate and symptoms.