Pulmonary Embolism: Symptoms, Causes, Treatment
What are the symptoms of a pulmonary embolism?
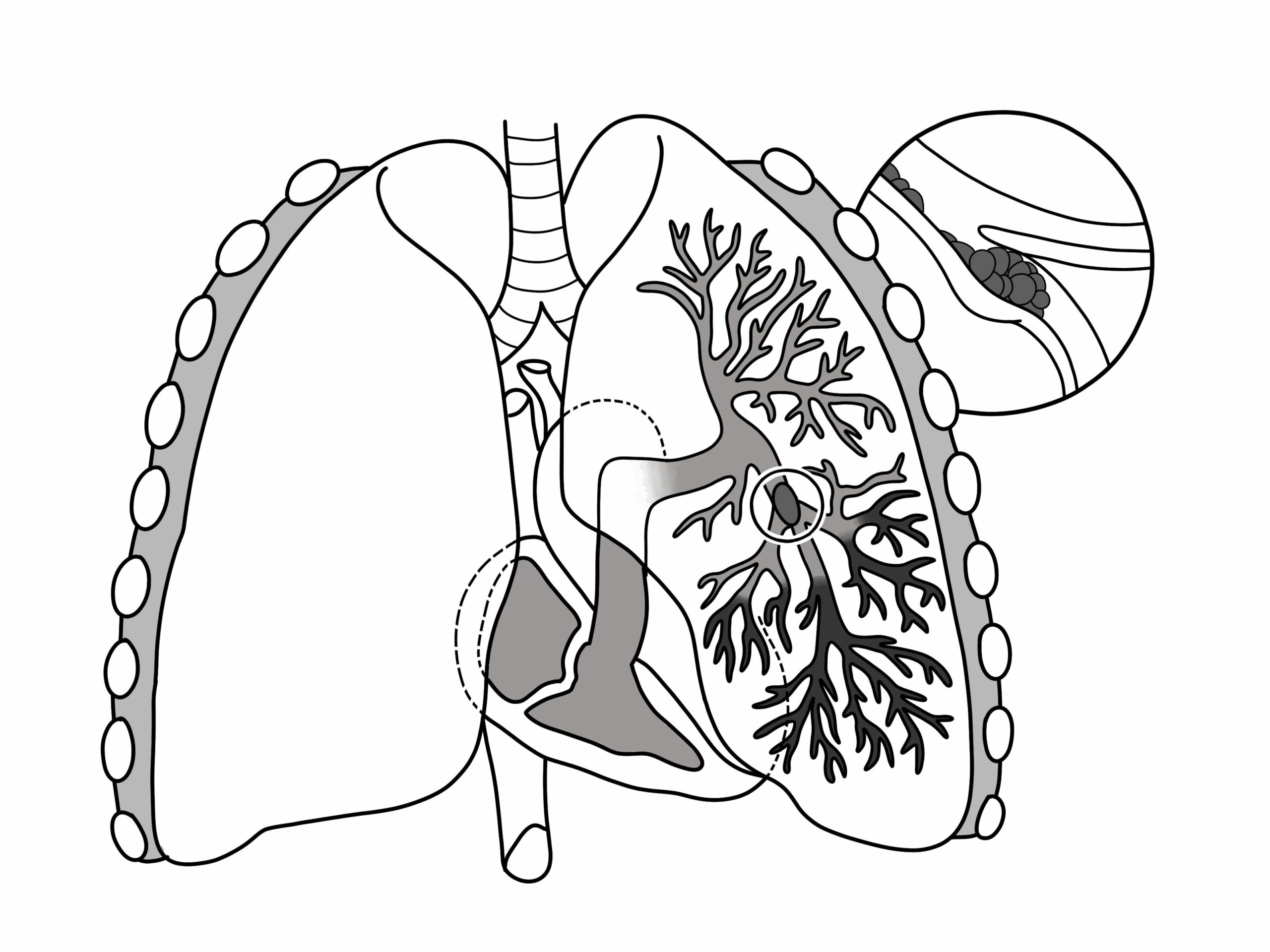
A pulmonary embolism (PE) occurs when a blood clot travels to the lungs and blocks a pulmonary artery or one of its branches. The symptoms of a pulmonary embolism can vary depending on the size of the clot and the extent of the blockage. Common symptoms include:
- Shortness of Breath: This is often the most common symptom and may occur suddenly or worsen over time. It may be mild or severe, and may be worse with exertion.
- Chest Pain: Chest pain or discomfort, which may feel like a sharp, stabbing pain that worsens with deep breaths, coughing, or movement. The pain may also be dull and constant.
- Cough: A cough that may produce bloody or blood-streaked sputum (hemoptysis).
- Rapid Heart Rate: A rapid or irregular heartbeat (palpitations).
- Feeling Lightheaded or Dizzy: This may occur with or without fainting.
- Excessive Sweating: Especially if accompanied by other symptoms.
- Leg Swelling: Swelling in one or both legs, usually in the calf, due to a deep vein thrombosis (DVT) that may have led to the pulmonary embolism.
It’s important to note that not everyone with a pulmonary embolism will experience all of these symptoms, and the severity of symptoms can vary. Some people may have no symptoms at all, especially if the clot is small or if there are underlying lung or heart conditions.
A pulmonary embolism is a serious condition that requires immediate medical attention. If you experience any symptoms of a pulmonary embolism, especially sudden onset of shortness of breath, chest pain, or coughing up blood, seek emergency medical care immediately.
What are the causes of a pulmonary embolism?
A pulmonary embolism (PE) occurs when a blood clot (thrombus) forms in a vein, usually in the deep veins of the legs (a condition known as deep vein thrombosis, or DVT), and then travels to the lungs, where it becomes lodged in a pulmonary artery or its branches. The main causes and risk factors for pulmonary embolism include:
- Deep Vein Thrombosis (DVT): The most common cause of pulmonary embolism is a blood clot that forms in a deep vein, usually in the legs. If a part of the clot breaks off, it can travel through the bloodstream to the lungs.
- Immobility: Prolonged periods of immobility, such as during long flights or car rides, bed rest, or hospitalization, can increase the risk of developing blood clots in the legs that can lead to pulmonary embolism.
- Surgery: Certain types of surgery, particularly orthopedic surgeries such as hip or knee replacement, can increase the risk of developing DVT and subsequent pulmonary embolism.
- Cancer: Cancer and cancer treatments can increase the risk of blood clots, as can the presence of a tumor that compresses blood vessels or affects blood flow.
- Pregnancy and Childbirth: Pregnancy and the postpartum period are associated with an increased risk of blood clots due to changes in hormone levels, increased pressure on the veins, and decreased mobility.
- Hormone Therapy and Birth Control Pills: Estrogen-containing medications, such as hormone replacement therapy and birth control pills, can increase the risk of blood clots.
- Obesity: Obesity is a risk factor for both DVT and pulmonary embolism.
- Smoking: Smoking damages the blood vessels and can increase the risk of blood clots.
- Certain Medical Conditions: Conditions such as heart disease, lung disease, and inflammatory disorders can increase the risk of blood clots.
- Inherited or Acquired Blood Disorders: Some people have an increased tendency to develop blood clots due to genetic factors or acquired conditions.
It’s important to note that while these are common causes and risk factors for pulmonary embolism, not everyone with these risk factors will develop the condition, and other factors may also contribute to the development of a pulmonary embolism.
What is the treatment for a pulmonary embolism?
Treatment for a pulmonary embolism (PE) aims to prevent the clot from growing larger, prevent new clots from forming, and reduce the risk of complications. The specific treatment approach depends on the severity of the PE and the individual’s overall health. Common treatments for PE include:
- Anticoagulant Medications: Also known as blood thinners, these medications are typically the first-line treatment for PE. They help prevent new clots from forming and existing clots from getting larger. Common anticoagulants include heparin, low molecular weight heparin (LMWH), and warfarin. Newer oral anticoagulants such as rivaroxaban, apixaban, and dabigatran are also used.
- Thrombolytic Therapy: In severe cases of PE where there is a large clot causing significant symptoms and hemodynamic instability, thrombolytic therapy may be used to dissolve the clot quickly. This treatment carries a higher risk of bleeding and is typically reserved for life-threatening cases.
- Surgical Embolectomy: In some cases, a surgical procedure known as an embolectomy may be performed to remove the clot from the pulmonary artery. This is typically reserved for cases where other treatments are not effective or cannot be used.
- Inferior Vena Cava (IVC) Filter: In cases where there is a high risk of recurrent PE and anticoagulant therapy is contraindicated or ineffective, an IVC filter may be placed in the inferior vena cava (the large vein that returns blood from the lower body to the heart) to catch clots before they reach the lungs.
- Oxygen Therapy: Supplemental oxygen may be given to improve oxygenation of the blood and relieve symptoms such as shortness of breath.
- Pain Management: Pain medications may be prescribed to relieve chest pain associated with PE.
- Compression Stockings: Compression stockings may be recommended to help prevent blood clots from forming in the legs.
- Lifestyle Changes: Making lifestyle changes such as quitting smoking, losing weight, and staying active can help reduce the risk of future blood clots.
It’s important to follow the treatment plan prescribed by your healthcare provider and attend follow-up appointments to monitor your condition. Prompt treatment of PE is crucial to prevent complications and improve outcomes.