Epididymitis: Symptoms, Causes, Treatment
What are the symptoms of epididymitis?
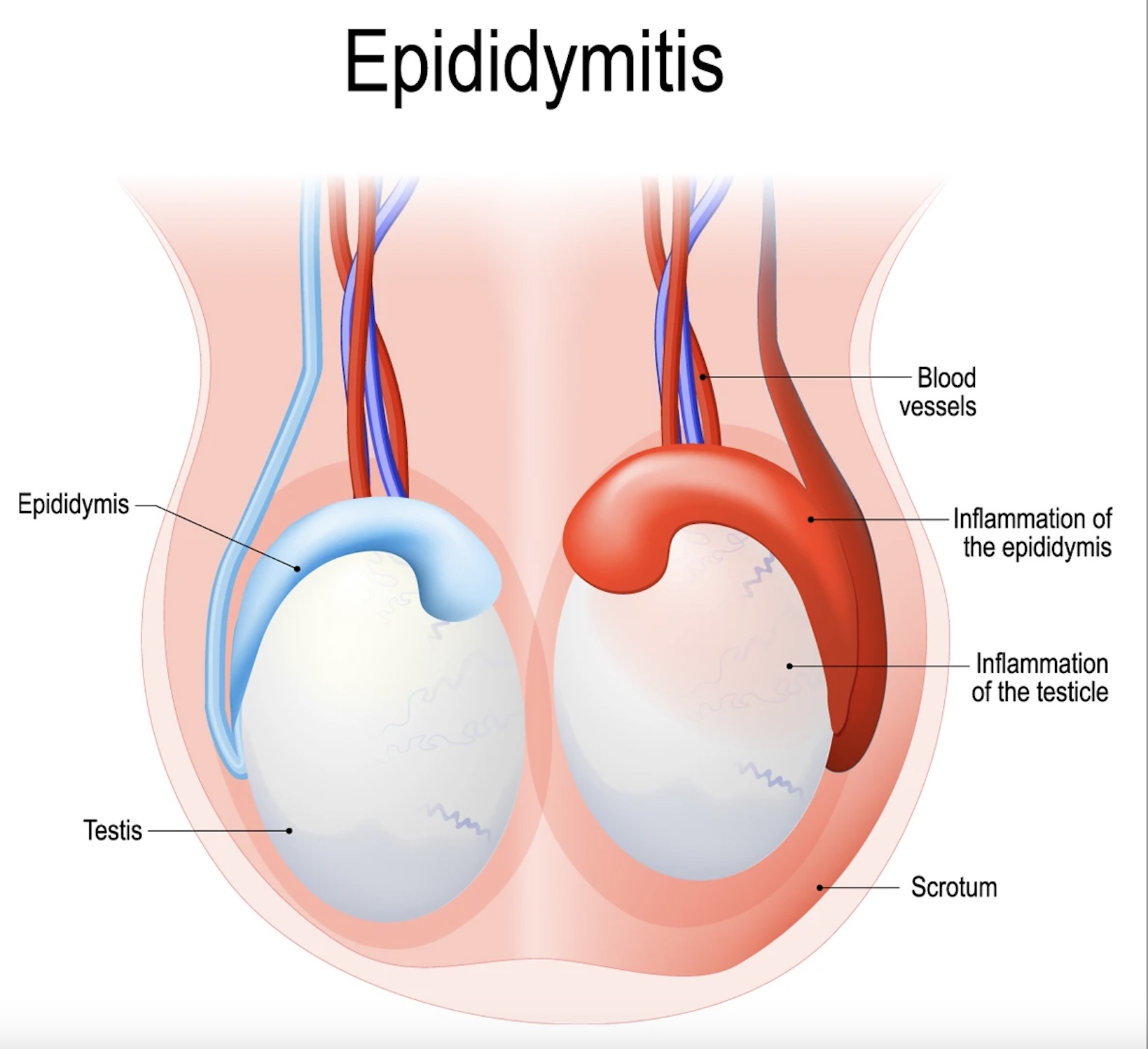
Epididymitis is the inflammation of the epididymis, a coiled tube located at the back of the testicle that stores and transports sperm. The symptoms of epididymitis can vary depending on the cause (e.g., bacterial infection, non-infectious inflammation) and may include:
- Pain and Tenderness: The most common symptom of epididymitis is pain and tenderness in one or both testicles. The pain may start gradually and intensify over time.
- Swelling: The affected testicle may become swollen and inflamed, leading to a noticeable enlargement of the scrotum.
- Redness and Warmth: The skin of the scrotum may appear red and feel warm to the touch due to inflammation.
- Fever and Chills: Some individuals with epididymitis may develop a fever, which may be accompanied by chills and sweating.
- Urinary Symptoms: In cases of sexually transmitted epididymitis, urinary symptoms such as burning or pain with urination, increased frequency of urination, or urgency to urinate may be present.
- Discharge: In cases of bacterial epididymitis, there may be a discharge from the penis, which may be clear or pus-like.
- Painful Ejaculation: Some individuals with epididymitis may experience pain or discomfort during ejaculation.
- Abdominal Pain: In some cases, the pain from epididymitis may radiate to the lower abdomen or groin area.
It’s important to see a healthcare provider if you experience symptoms of epididymitis, especially if they are severe or persistent. Prompt treatment is important to prevent complications and relieve symptoms.
What are the causes of epididymitis?
Epididymitis can have several causes, including infectious and non-infectious factors. The most common causes of epididymitis include:
- Bacterial Infection: The most common cause of epididymitis is a bacterial infection, which can be either sexually transmitted (e.g., gonorrhea, chlamydia) or non-sexually transmitted (e.g., urinary tract infection, prostate infection). Bacteria can travel from the urethra or bladder to the epididymis, leading to inflammation.
- Non-Bacterial Inflammation: In some cases, epididymitis may be caused by non-infectious factors, such as trauma, autoimmune disorders, or chemical irritation. This type of epididymitis is less common than bacterial epididymitis.
- Urinary Tract Procedures: Procedures involving the urinary tract, such as catheterization or prostate biopsy, can sometimes introduce bacteria into the urinary tract, leading to epididymitis.
- Reflux of Urine: Reflux of urine from the bladder into the ejaculatory ducts and epididymis, known as urinary reflux, can lead to inflammation and infection.
- Sexually Transmitted Infections: Sexually transmitted infections (STIs) such as gonorrhea and chlamydia can cause epididymitis, especially in sexually active men.
- Urethral Stricture: A urethral stricture, which is a narrowing of the urethra, can lead to urinary retention and increase the risk of infection and inflammation in the epididymis.
- Physical Activity: Strenuous physical activity or trauma to the scrotum can sometimes lead to epididymitis, although this is less common.
- Anatomical Abnormalities: Some men may have anatomical abnormalities that increase the risk of epididymitis, such as congenital abnormalities or previous surgery in the genital or urinary tract.
It’s important to see a healthcare provider for an accurate diagnosis and appropriate treatment if you experience symptoms of epididymitis. Treatment will depend on the underlying cause and may include antibiotics, pain management, and other supportive measures.
What is the treatment for epididymitis?
The treatment for epididymitis depends on the underlying cause (e.g., bacterial infection, non-infectious inflammation) and severity of symptoms. In most cases, epididymitis is treated with a combination of antibiotics, pain management, and supportive measures. Here are some common treatment approaches for epididymitis:
- Antibiotics: If epididymitis is caused by a bacterial infection, antibiotics are usually prescribed to treat the infection. The choice of antibiotic depends on the suspected or identified bacteria and the severity of the infection. It’s important to complete the full course of antibiotics as prescribed by your healthcare provider.
- Pain Management: Over-the-counter pain medications, such as ibuprofen or acetaminophen, may be recommended to relieve pain and discomfort associated with epididymitis. In some cases, your healthcare provider may prescribe stronger pain medications.
- Rest and Elevation: Resting and elevating the scrotum with a supportive undergarment (e.g., jockstrap) can help reduce swelling and discomfort.
- Ice Packs: Applying ice packs to the scrotum for 15-20 minutes several times a day can help reduce swelling and pain.
- Hydration: Drinking plenty of fluids can help flush out bacteria and reduce the risk of urinary tract infections, which can contribute to epididymitis.
- Avoidance of Irritants: Avoiding activities that may irritate the scrotum, such as biking or heavy lifting, can help reduce discomfort and promote healing.
- Treatment of Underlying Conditions: If epididymitis is caused by underlying conditions, such as a urinary tract infection or sexually transmitted infection, those conditions will also need to be treated.
In some cases, especially if symptoms are severe or do not improve with conservative treatment, additional interventions may be necessary. These may include drainage of any abscesses, surgical correction of anatomical abnormalities, or other procedures to relieve symptoms and prevent complications.
It’s important to see a healthcare provider for an accurate diagnosis and appropriate treatment if you experience symptoms of epididymitis. Prompt treatment can help relieve symptoms, prevent complications, and reduce the risk of recurrence.