Interstitial Lung Disease: Symptoms, Causes & Treatment
What are the symptoms of interstitial lung disease?
Interstitial lung disease (ILD) refers to a group of lung disorders that cause inflammation and scarring (fibrosis) of the interstitium, which is the tissue that surrounds and supports the air sacs (alveoli) in the lungs. The symptoms of ILD can vary depending on the specific type of ILD and the extent of lung damage, but common symptoms may include:
- Shortness of breath: Shortness of breath (dyspnea) is a common symptom of ILD. It may start gradually and worsen over time, particularly with physical activity.
- Dry cough: A persistent, dry cough is another common symptom of ILD. The cough may be mild at first but can become more frequent and severe as the disease progresses.
- Fatigue: Fatigue is a common symptom of ILD and can be caused by the body’s increased effort to breathe due to reduced lung function.
- Weakness: Weakness and muscle fatigue may occur due to the increased effort required to breathe and the decreased oxygen levels in the blood.
- Clubbing of the fingers or toes: In some cases of ILD, the fingertips and toes may become rounded and wider at the tips (clubbing). This is thought to be due to low oxygen levels in the blood over a long period of time.
- Chest discomfort or tightness: Some people with ILD may experience chest discomfort or a feeling of tightness in the chest.
- Unintentional weight loss: Weight loss may occur in some cases of ILD, particularly as the disease progresses and the body has to work harder to breathe.
- Cyanosis: In severe cases of ILD, the skin and lips may take on a bluish tint (cyanosis) due to low oxygen levels in the blood.
It’s important to note that the symptoms of ILD can be similar to those of other lung and respiratory conditions, so a thorough evaluation by a healthcare provider is necessary to determine the underlying cause of symptoms.
What are the causes of interstitial lung disease?
Interstitial lung disease (ILD) refers to a group of lung disorders characterized by inflammation and scarring (fibrosis) of the interstitium, which is the tissue that surrounds and supports the air sacs (alveoli) in the lungs. The exact cause of ILD is often unknown, but several factors and conditions can contribute to its development. These include:
- Idiopathic interstitial pneumonias (IIPs): This group of ILDs includes idiopathic pulmonary fibrosis (IPF), which is the most common and most severe form of IIP. The cause of IIPs is unknown, but they are thought to result from a combination of genetic and environmental factors.
- Connective tissue diseases: ILD can occur in association with certain autoimmune diseases, such as rheumatoid arthritis, systemic sclerosis (scleroderma), and systemic lupus erythematosus. In these cases, ILD is thought to result from an abnormal immune response that causes inflammation and fibrosis in the lungs.
- Environmental and occupational exposures: Exposure to certain environmental and occupational hazards can increase the risk of developing ILD. These include exposure to asbestos, silica dust, coal dust, and various other airborne pollutants and toxins.
- Drug-induced ILD: Some medications, particularly certain chemotherapy drugs, antibiotics, and anti-inflammatory drugs, can cause ILD as a side effect. ILD caused by medications is typically reversible once the medication is stopped.
- Infections: Certain infections, such as viral infections (e.g., Epstein-Barr virus, cytomegalovirus) and fungal infections (e.g., Histoplasma, Aspergillus), can lead to ILD, particularly in people with weakened immune systems.
- Genetic factors: In some cases, genetic factors may play a role in the development of ILD. Mutations in certain genes have been associated with an increased risk of ILD, although the exact mechanisms are not well understood.
It’s important to note that the underlying cause of ILD can vary widely among individuals, and in many cases, the cause remains unknown. A thorough evaluation by a healthcare provider is necessary to determine the underlying cause of ILD and to develop an appropriate treatment plan.
What is the treatment for interstitial lung disease?
The treatment for interstitial lung disease (ILD) depends on the underlying cause and the specific type of ILD. The goals of treatment are to reduce inflammation, slow the progression of fibrosis (scarring), manage symptoms, and improve quality of life. Treatment options for ILD may include:
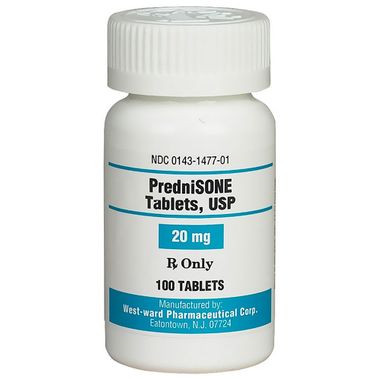
- Corticosteroids: Corticosteroids, such as prednisone, may be prescribed to reduce inflammation in the lungs and slow the progression of fibrosis. However, long-term use of corticosteroids can have significant side effects, so they are typically used for short periods or at low doses.
- Immunosuppressive medications: In some cases, medications that suppress the immune system, such as azathioprine, mycophenolate, or cyclophosphamide, may be used to reduce inflammation and fibrosis in the lungs.
- Antifibrotic medications: For certain types of ILD, such as idiopathic pulmonary fibrosis (IPF), antifibrotic medications like pirfenidone or nintedanib may be prescribed to slow the progression of fibrosis.
- Oxygen therapy: Supplemental oxygen therapy may be necessary if ILD causes low levels of oxygen in the blood. Oxygen therapy can help improve breathing and reduce symptoms such as shortness of breath.
- Pulmonary rehabilitation: Pulmonary rehabilitation programs can help improve lung function, reduce symptoms, and improve quality of life through exercise, education, and support.
- Lung transplant: In severe cases of ILD that do not respond to other treatments, lung transplantation may be considered. A lung transplant can improve quality of life and increase life expectancy for some people with ILD.
- Supportive care: Supportive care, such as nutritional support, counseling, and medications to manage symptoms like cough or pain, may also be part of the treatment plan for ILD.
It’s important for individuals with ILD to work closely with a healthcare team, which may include pulmonologists, rheumatologists, and other specialists, to develop a personalized treatment plan. Regular monitoring and follow-up are essential to assess the effectiveness of treatment and make any necessary adjustments.