HER2-Positive Breast Cancer: Symptoms, Causes, Treatment
What are the symptoms of HER2-positive breast cancer?
HER2-positive breast cancer is a subtype of breast cancer that is characterized by the overexpression of a protein called human epidermal growth factor receptor 2 (HER2). Symptoms of HER2-positive breast cancer are similar to those of other types of breast cancer and may include:
- Lump or mass in the breast: This is often the most noticeable symptom of breast cancer. The lump may feel hard, irregular in shape, and different from the surrounding breast tissue.
- Changes in breast size or shape: The breast may become larger or more swollen, or there may be a change in the shape of the breast.
- Changes in the skin: The skin of the breast may become red, swollen, or dimpled, resembling the texture of an orange peel.
- Nipple changes: The nipple may become inverted (turned inward) or change in shape or position. There may also be discharge from the nipple, especially if it is bloody.
- Breast pain or discomfort: While breast cancer is not usually painful in the early stages, some women may experience breast pain or discomfort.
- Swollen lymph nodes: Lymph nodes under the arm or around the collarbone may become swollen or tender.
It’s important to note that these symptoms can also be caused by conditions other than breast cancer. If you notice any changes in your breasts or have any concerns, it’s important to see a healthcare provider for a thorough evaluation. Early detection and treatment of breast cancer, including HER2-positive breast cancer, can improve outcomes.
What are the causes of HER2-positive breast cancer?
The exact cause of HER2-positive breast cancer is not fully understood, but several factors are believed to play a role in its development. These factors include:
- HER2 gene amplification: In HER2-positive breast cancer, there is an overexpression of the human epidermal growth factor receptor 2 (HER2) protein, which is encoded by the HER2 gene. This overexpression is often due to a gene amplification, where multiple copies of the HER2 gene are present in the cancer cells.
- Hormone receptor status: HER2-positive breast cancer is often hormone receptor-negative, meaning that the cancer cells do not have receptors for the hormones estrogen and progesterone. This is in contrast to hormone receptor-positive breast cancers, which do have these receptors.
- Genetic mutations: Mutations in certain genes, such as the BRCA1 and BRCA2 genes, can increase the risk of developing breast cancer, including HER2-positive breast cancer.
- Environmental factors: Factors such as exposure to radiation, certain chemicals, and lifestyle factors like smoking and alcohol consumption may also play a role in the development of HER2-positive breast cancer.
- Family history: Having a family history of breast cancer, especially in first-degree relatives (such as a mother, sister, or daughter), can increase the risk of developing HER2-positive breast cancer.
It’s important to note that while these factors may increase the risk of developing HER2-positive breast cancer, not all women with these risk factors will develop the disease. Conversely, some women with no known risk factors may still develop HER2-positive breast cancer.
What is the treatment for HER2-positive breast cancer?
The treatment for HER2-positive breast cancer typically involves a combination of therapies, which may include:
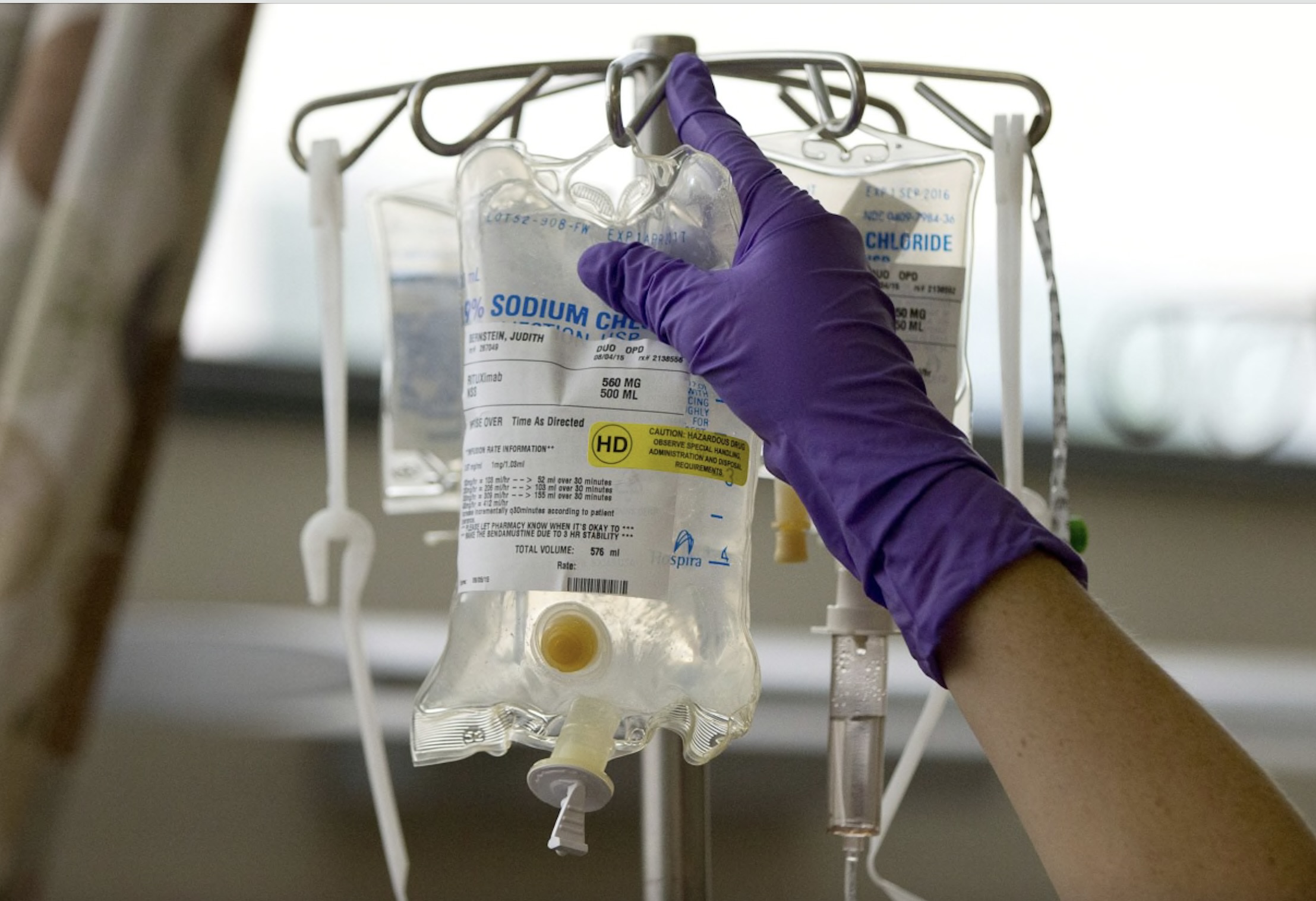
- Targeted therapy: HER2-positive breast cancer is treated with drugs that specifically target the HER2 protein, such as trastuzumab (Herceptin), pertuzumab (Perjeta), and ado-trastuzumab emtansine (Kadcyla). These drugs can help slow or stop the growth of cancer cells.
- Chemotherapy: Chemotherapy may be used in combination with targeted therapy to help shrink the tumor before surgery (neoadjuvant chemotherapy) or to kill any remaining cancer cells after surgery (adjuvant chemotherapy).
- Hormone therapy: If the cancer is also hormone receptor-positive, hormone therapy drugs such as tamoxifen or aromatase inhibitors may be used to block the effects of estrogen on the cancer cells.
- Surgery: Surgery may be used to remove the tumor (lumpectomy) or the entire breast (mastectomy). In some cases, surgery may be followed by radiation therapy to help destroy any remaining cancer cells.
- Radiation therapy: Radiation therapy uses high-energy beams to kill cancer cells. It may be used after surgery to destroy any remaining cancer cells in the breast or lymph nodes.
- Clinical trials: Participation in clinical trials may be an option for some patients. These trials test new treatments or combinations of treatments to determine their safety and effectiveness.
The specific treatment plan for HER2-positive breast cancer will depend on several factors, including the stage of the cancer, the presence of hormone receptors, and the patient’s overall health and preferences. A multidisciplinary team of healthcare providers, including oncologists, surgeons, and other specialists, will work together to develop a treatment plan that is tailored to the individual needs of each patient.