Lichen Ruber Planus: Symptoms, Causes, Treatment
What are the symptoms of lichen ruber planus?
Lichen ruber planus, commonly known as lichen planus, is a chronic inflammatory skin condition that can affect the skin, mucous membranes, nails, and hair. The symptoms of lichen planus can vary depending on the area of the body affected, but common symptoms include:
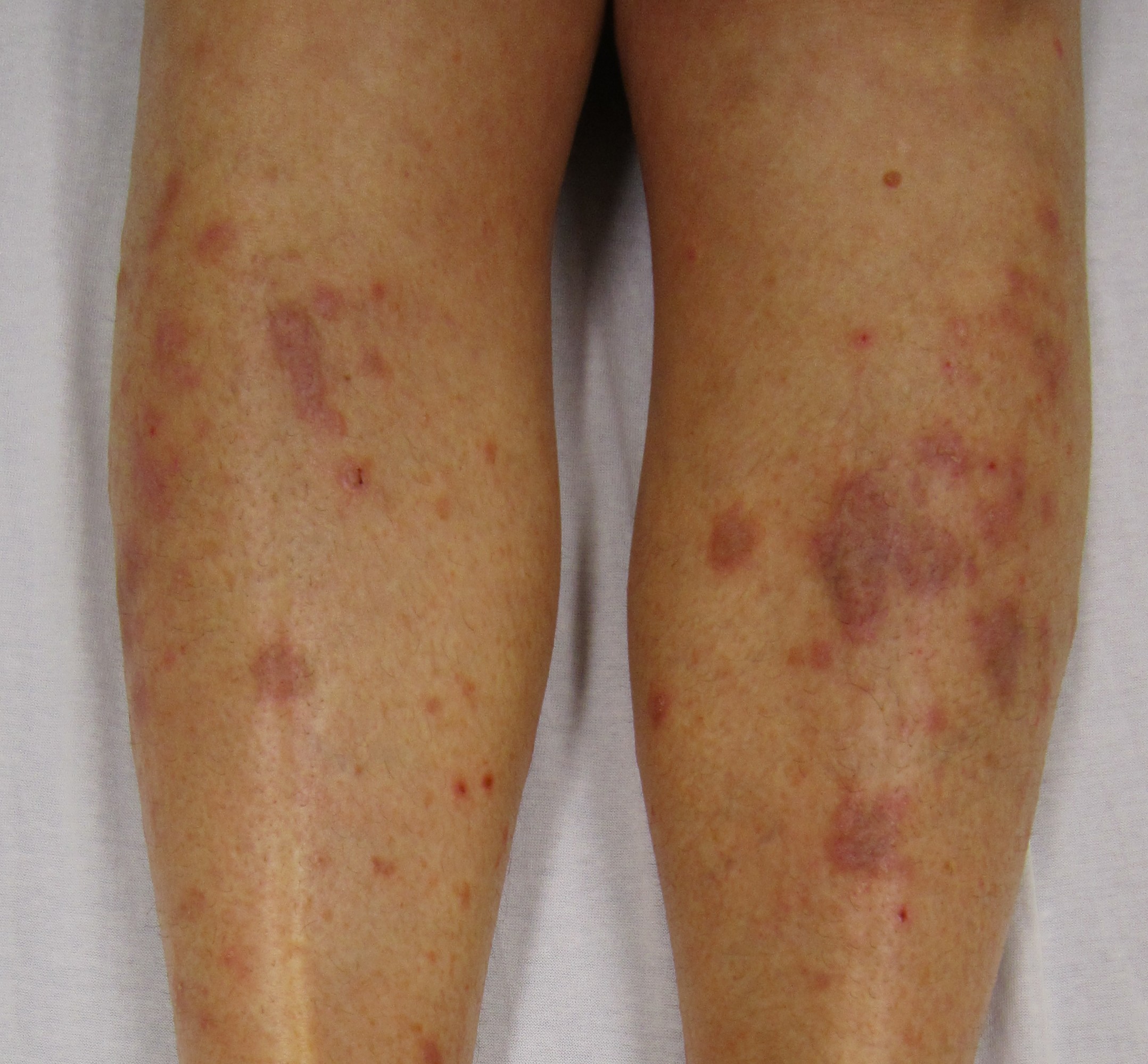
- Skin lesions: The hallmark symptom of lichen planus is the presence of small, flat-topped, polygonal bumps on the skin. These bumps may be shiny and have a reddish-purple color. They often have a distinct pattern of fine white lines called Wickham’s striae.
- Itching (pruritus): The affected skin may be itchy, and scratching can lead to the development of open sores or scabs.
- Nail changes: Lichen planus can cause changes to the nails, including thinning, ridges, grooves, and splitting. The nails may also become brittle or discolored.
- Mucous membrane involvement: In some cases, lichen planus can affect the mucous membranes, such as those in the mouth, genitals, or esophagus. Oral lichen planus can cause white, lacy patches on the inside of the cheeks, gums, or tongue. Genital lichen planus can cause itching, burning, and painful sores.
- Hair loss: Lichen planus can cause scarring alopecia, a form of hair loss where the hair follicles are permanently damaged and replaced with scar tissue. This can lead to permanent hair loss in the affected area.
- Koebner phenomenon: Some individuals with lichen planus may experience the Koebner phenomenon, where new lesions develop at the site of skin injury or trauma.
- Symmetrical distribution: Lichen planus lesions often appear symmetrically on the body, meaning they occur in the same location on both sides of the body.
It’s important to note that the symptoms of lichen planus can vary widely from person to person, and not everyone with the condition will experience all of these symptoms. If you suspect you have lichen planus or are experiencing symptoms, it’s important to see a dermatologist or healthcare professional for an accurate diagnosis and appropriate treatment.
What are the causes of lichen ruber planus?
The exact cause of lichen planus is not well understood, but it is believed to be an autoimmune disorder in which the body’s immune system mistakenly attacks healthy skin cells, mucous membranes, nails, or hair follicles. Several factors may contribute to the development of lichen planus, including:
- Autoimmune factors: Lichen planus is thought to be an autoimmune disorder, similar to other autoimmune conditions. In autoimmune disorders, the immune system mistakenly attacks healthy tissues, leading to inflammation and tissue damage.
- Genetic factors: There may be a genetic predisposition to developing lichen planus, as the condition can sometimes run in families. Certain genetic variations may increase the risk of developing autoimmune disorders like lichen planus.
- Environmental factors: Certain environmental factors, such as infections, medications, or chemicals, may trigger the development of lichen planus in susceptible individuals. Common triggers include hepatitis C virus infection, certain medications (such as beta-blockers, nonsteroidal anti-inflammatory drugs, and certain antibiotics), and exposure to certain chemicals or metals.
- Stress: Some researchers believe that stress may play a role in triggering or exacerbating lichen planus in some individuals, although the exact relationship is not well understood.
- Other factors: Lichen planus has been associated with other medical conditions, such as hepatitis C virus infection, diabetes, and certain autoimmune diseases, suggesting a complex interplay of factors in the development of the condition.
It’s important to note that while these factors may contribute to the development of lichen planus, the exact cause of the condition is not well understood. Further research is needed to fully understand the underlying mechanisms of lichen planus and to develop more effective treatments. If you have been diagnosed with lichen planus, it’s important to work closely with a dermatologist or healthcare professional to manage the condition and any underlying factors that may be contributing to it.
What is the treatment for lichen ruber planus?
The treatment for lichen ruber planus (lichen planus) aims to reduce symptoms, prevent complications, and improve the appearance of the skin, mucous membranes, nails, or hair. Treatment options for lichen planus may include:
- Topical corticosteroids: Topical corticosteroid creams or ointments are often used as first-line treatment for lichen planus to reduce inflammation and itching. These medications are applied directly to the affected skin.
- Topical calcineurin inhibitors: Tacrolimus (Protopic) and pimecrolimus (Elidel) are topical medications that suppress the immune response and can be used to treat lichen planus, especially in sensitive areas such as the genitals or mucous membranes.
- Oral corticosteroids: In severe cases of lichen planus that do not respond to other treatments, oral corticosteroids may be prescribed to help reduce inflammation and itching. However, long-term use of oral corticosteroids is generally not recommended due to the risk of side effects.
- Systemic retinoids: Oral retinoid medications, such as acitretin, may be prescribed to help normalize skin cell growth and reduce inflammation in lichen planus.
- Phototherapy: Phototherapy, or light therapy, involves exposing the affected skin to ultraviolet (UV) light to reduce inflammation and improve symptoms. This treatment is often used in combination with other therapies for lichen planus.
- Antihistamines: Oral antihistamines may be prescribed to help relieve itching associated with lichen planus.
- Intralesional corticosteroid injections: In some cases, corticosteroids may be injected directly into the lesions to help reduce inflammation and improve symptoms.
- Mucous membrane treatments: For lichen planus affecting the mucous membranes, treatments may include topical corticosteroids, oral medications, or oral rinses to reduce inflammation and relieve symptoms.
- Nail treatments: For lichen planus affecting the nails, treatments may include topical corticosteroids, intralesional corticosteroid injections, or systemic medications to improve nail health.
It’s important to work closely with a dermatologist or healthcare professional to develop a treatment plan that is tailored to your specific needs and symptoms. Lichen planus is a chronic condition, and treatment may need to be continued long-term to effectively manage symptoms and prevent complications.