Plasmapheresis: Risks & Benefits
How does plasmapheresis work?
Plasmapheresis is a medical procedure used to treat certain autoimmune disorders, neurological conditions, and other medical conditions. It involves removing blood from the body, separating the plasma (the liquid portion of the blood) from the blood cells, and then returning the blood cells to the body. Here’s how the process typically works:
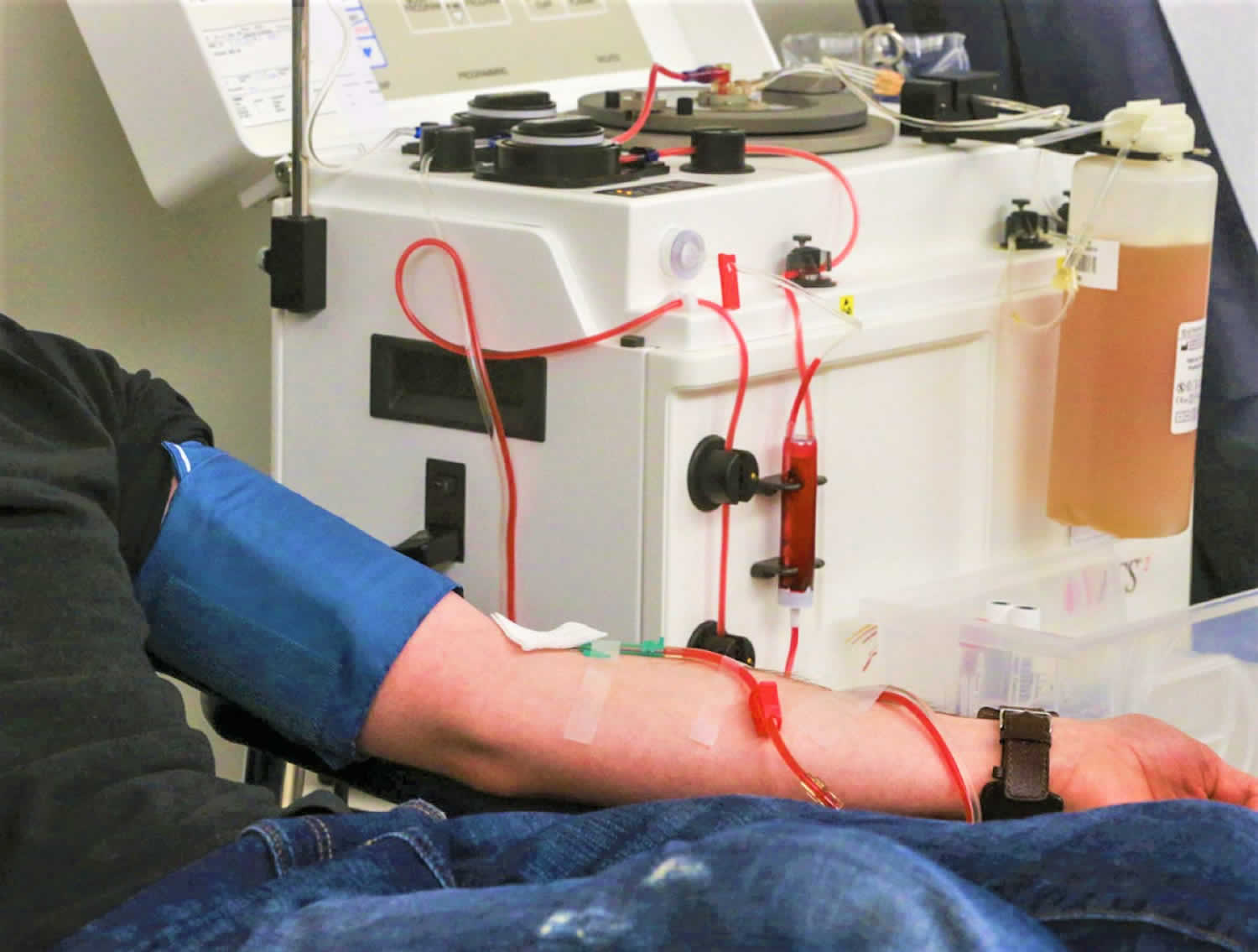
- Preparation: Before the procedure, a healthcare provider will insert a needle into a vein, usually in the arm, to access the bloodstream. This needle is connected to a machine called a plasmapheresis unit.
- Blood removal: The plasmapheresis unit draws blood from the vein and passes it through a series of tubes into a centrifuge or a plasma separator. In the centrifuge, the blood is spun at high speeds, which separates the plasma from the blood cells.
- Plasma separation: Once the plasma is separated, it is collected in a bag or container, while the blood cells are returned to the body through the same needle or a separate needle in the other arm.
- Replacement fluid: In some cases, a replacement fluid, such as albumin or saline, may be infused into the bloodstream to help maintain blood volume and electrolyte balance.
- Completion: The procedure typically takes a few hours to complete, depending on the amount of plasma that needs to be removed. After the procedure, the needle is removed, and the access site is bandaged.
Plasmapheresis is thought to work by removing harmful antibodies, immune complexes, and other substances from the plasma that contribute to the underlying condition. It can help reduce symptoms and improve outcomes in certain conditions, but it is not a cure and may need to be repeated periodically depending on the condition being treated.
What are the risks of plasmapheresis?
Plasmapheresis is generally considered safe, but like any medical procedure, it carries some risks. Some potential risks of plasmapheresis include:
- Low blood pressure: Plasmapheresis can temporarily lower blood pressure, which may cause dizziness, lightheadedness, or fainting.
- Infection: There is a small risk of infection at the site where the needle is inserted into the vein. This risk is higher in individuals with weakened immune systems such as HIV infected persons.
- Bleeding: Plasmapheresis involves inserting a needle into a vein, which can sometimes cause bleeding or bruising at the insertion site.
- Allergic reaction: Some people may have an allergic reaction to the replacement fluid or anticoagulant medications used during plasmapheresis. Symptoms of an allergic reaction may include hives, itching, or difficulty breathing.
- Clotting of the catheter: In some cases, the catheter used to access the bloodstream can become blocked or clot, which may require removal or replacement.
- Electrolyte imbalances: Plasmapheresis can cause changes in electrolyte levels, such as low calcium or magnesium levels, which can lead to muscle cramps, weakness, or other symptoms.
- Hypocalcemia: Removal of plasma can lead to a drop in calcium levels in the blood, which can cause symptoms such as muscle spasms, numbness or tingling in the fingers and toes, and seizures.
- Hypovolemia: Plasmapheresis can lead to a decrease in blood volume, which can cause symptoms such as dizziness, weakness, and low blood pressure.
- Nerve damage: There is a small risk of nerve damage at the insertion site or due to pressure from the catheter.
- Fluid overload: In rare cases, too much replacement fluid may be infused, leading to fluid overload and potentially causing swelling, shortness of breath, or heart problems.
It’s important to discuss the potential risks and benefits of plasmapheresis with your healthcare provider before undergoing the procedure. The risks can vary depending on the individual’s health status and the specific condition being treated.
What are the benefits of plasmapheresis?
Plasmapheresis can offer several benefits for individuals with certain medical conditions. Some potential benefits include:
- Removal of harmful substances: Plasmapheresis can effectively remove harmful antibodies, immune complexes, toxins, and other substances from the plasma that may be contributing to the underlying condition.
- Reduction of symptoms: By removing these harmful substances, plasmapheresis can help reduce symptoms associated with autoimmune disorders, neurological conditions, and other medical conditions. This can lead to improved quality of life for individuals with these conditions.
- Treatment of acute conditions: Plasmapheresis can be used to treat acute and severe conditions, such as Guillain-Barré syndrome, myasthenia gravis, and certain types of kidney disorders, where rapid removal of harmful substances from the plasma is necessary.
- Adjunct to other treatments: Plasmapheresis can be used as an adjunct to other treatments, such as immunosuppressive medications or chemotherapy, to help improve their effectiveness.
- Temporary relief: In some cases, plasmapheresis may provide temporary relief of symptoms, allowing time for other treatments to take effect or for the underlying condition to improve.
- Preparation for transplant: Plasmapheresis can be used to remove antibodies in individuals who are preparing for organ or stem cell transplantation, reducing the risk of rejection.
- Management of certain conditions: Plasmapheresis may be used as a long-term management strategy for certain chronic conditions, such as certain types of autoimmune disorders, to help maintain disease control and reduce symptoms.
It’s important to note that the benefits of plasmapheresis can vary depending on the individual’s health status, the specific condition being treated, and other factors. It’s essential to discuss the potential benefits and risks of plasmapheresis with your healthcare provider to determine if it is an appropriate treatment option for you.