Felty’s Syndrome: Symptoms, Causes, Treatment
What are the symptoms of Felty’s syndrome?
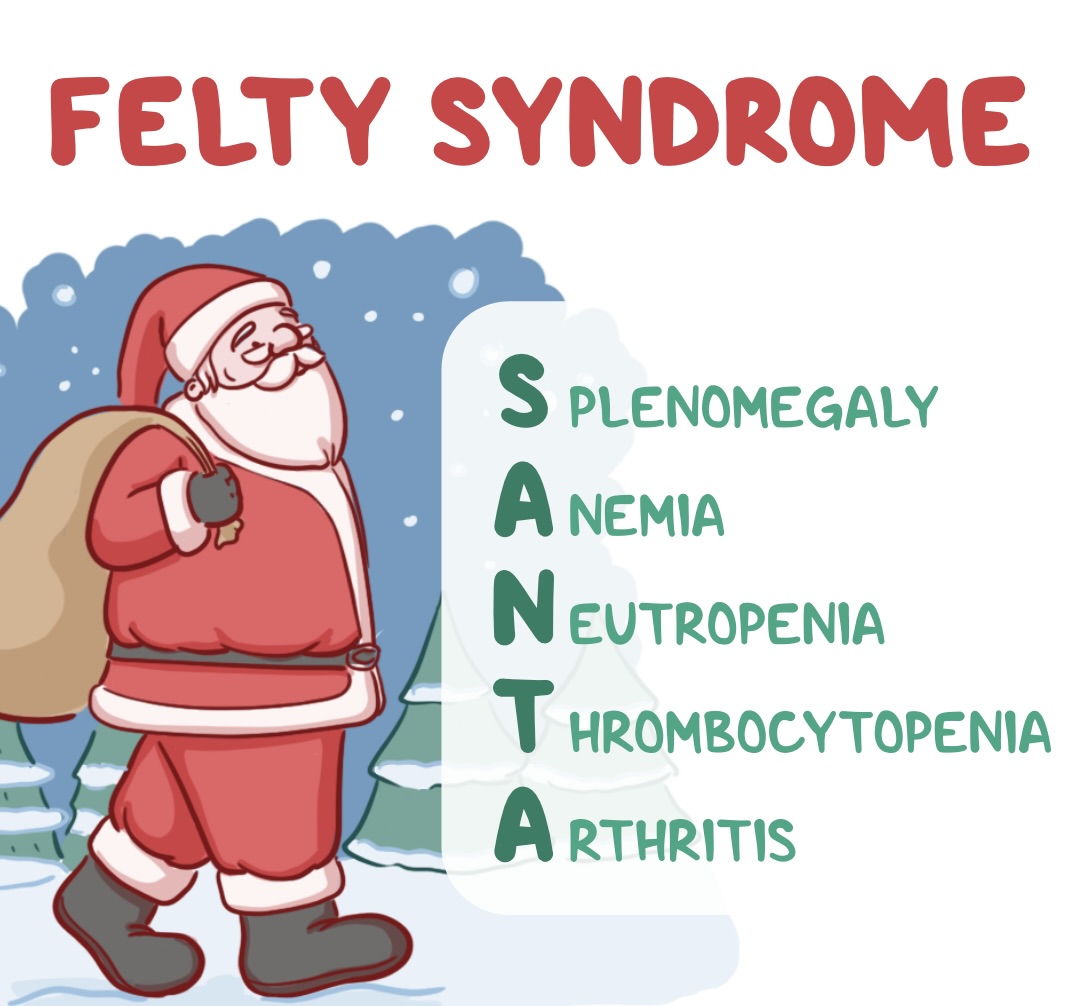
Felty’s syndrome is a rare complication of long-standing rheumatoid arthritis (RA). It is characterized by the presence of three conditions: rheumatoid arthritis, an enlarged spleen (splenomegaly), and a low white blood cell count (neutropenia). The symptoms of Felty’s syndrome can vary but may include:
- Rheumatoid arthritis symptoms: Felty’s syndrome is typically seen in individuals who have had RA for many years. Symptoms of RA include joint pain, swelling, stiffness, and inflammation. These symptoms can affect the hands, feet, knees, ankles, and other joints.
- Enlarged spleen: Splenomegaly, or an enlarged spleen, is a common feature of Felty’s syndrome. An enlarged spleen can cause discomfort or pain in the upper left side of the abdomen.
- Low white blood cell count: Neutropenia, or a low white blood cell count, is another characteristic feature of Felty’s syndrome. Neutrophils are a type of white blood cell that helps the body fight infections. A low neutrophil count can increase the risk of infections.
- Fatigue: Many people with Felty’s syndrome experience fatigue, which can be severe and debilitating.
- Recurrent infections: Due to the low white blood cell count, individuals with Felty’s syndrome are more susceptible to infections, especially bacterial infections.
- Weight loss: Some people with Felty’s syndrome may experience unintentional weight loss.
- Fever: Low-grade fever may occur, especially if there is an underlying infection.
It’s important to note that not all individuals with Felty’s syndrome will experience all of these symptoms, and the severity of symptoms can vary. Felty’s syndrome is a serious condition that requires careful management by a healthcare provider, usually a rheumatologist. Treatment aims to manage symptoms, reduce inflammation, and prevent infections. Treatment may include medications to suppress the immune system, such as disease-modifying antirheumatic drugs (DMARDs) or biologic agents, as well as medications to stimulate white blood cell production. In some cases, surgery to remove the spleen (splenectomy) may be considered.
What are the causes of Felty’s syndrome?
The exact cause of Felty’s syndrome is not well understood, but it is believed to be related to chronic inflammation and immune system dysfunction associated with rheumatoid arthritis (RA). Felty’s syndrome is considered a rare complication of RA, occurring in less than 1% of individuals with RA.
Several factors may contribute to the development of Felty’s syndrome, including:
- Chronic inflammation: RA is characterized by chronic inflammation in the joints, which can lead to the destruction of cartilage and bone. This chronic inflammation may also affect other organs, including the spleen.
- Autoimmune reaction: RA is an autoimmune disease, which means that the immune system mistakenly attacks the body’s own tissues. In Felty’s syndrome, the immune system may also attack the spleen and white blood cells, leading to splenomegaly and neutropenia.
- Genetic factors: There may be genetic factors that predispose some individuals with RA to develop Felty’s syndrome, although specific genetic markers have not been identified.
- Environmental factors: Environmental factors, such as infections or exposure to certain substances, may trigger or exacerbate the immune response in susceptible individuals.
- Other factors: Other factors, such as age and disease duration, may also play a role in the development of Felty’s syndrome. Felty’s syndrome is more common in older individuals with long-standing RA.
Overall, Felty’s syndrome is thought to be a complex interplay of genetic, environmental, and immunological factors. More research is needed to fully understand the mechanisms underlying this rare condition.
What is the treatment for Felty’s syndrome?
The treatment for Felty’s syndrome aims to manage symptoms, reduce inflammation, and prevent infections. Treatment is typically directed by a rheumatologist, who specializes in arthritis and autoimmune conditions. Treatment options for Felty’s syndrome may include:
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs, such as methotrexate, sulfasalazine, or leflunomide, are often used to reduce inflammation and slow the progression of rheumatoid arthritis in individuals with Felty’s syndrome.
- Biologic agents: Biologic agents, such as tumor necrosis factor (TNF) inhibitors (e.g., etanercept, adalimumab) or other biologic therapies (e.g., rituximab, tocilizumab), may be prescribed for individuals with Felty’s syndrome who do not respond adequately to DMARDs. These medications target specific components of the immune system involved in the inflammatory process.
- Corticosteroids: Corticosteroids, such as prednisone, may be used to reduce inflammation and suppress the immune response in individuals with Felty’s syndrome. However, long-term use of corticosteroids is generally avoided due to the risk of side effects.
- Splenectomy: In some cases, surgical removal of the spleen (splenectomy) may be considered for individuals with Felty’s syndrome who have severe neutropenia or recurrent infections despite medical treatment. Splenectomy can help improve white blood cell counts and reduce the risk of infections, but it is usually reserved for individuals who do not respond to other treatments.
- Growth factors: In some cases, medications that stimulate the production of white blood cells, such as granulocyte colony-stimulating factor (G-CSF), may be used to help increase neutrophil counts and reduce the risk of infections.
- Infection prevention: Due to the increased risk of infections in individuals with Felty’s syndrome, it is important to take steps to prevent infections. This may include receiving recommended vaccinations, practicing good hygiene, and avoiding exposure to sick individuals.
The treatment approach for Felty’s syndrome is individualized based on the severity of symptoms, the presence of complications, and the response to treatment. Regular monitoring and follow-up with a healthcare provider are important to ensure that the treatment plan is effective and to address any new or worsening symptoms.