Advance Directives
What are advance directives?
Advance directives are legal documents that allow individuals to express their wishes regarding medical treatment and healthcare decisions in the event that they are unable to communicate their preferences due to illness or incapacity. Advance directives are used to ensure that a person’s healthcare wishes are respected and followed by healthcare providers and family members.
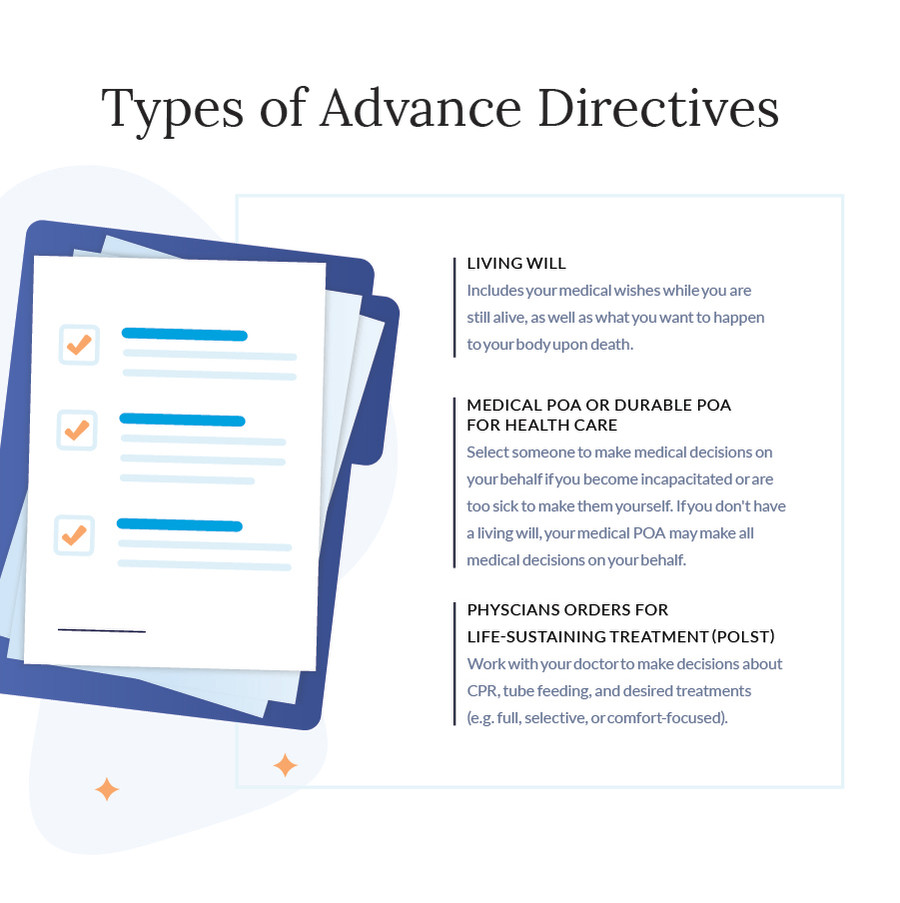
There are several types of advance directives, including:
- Living will: A living will is a document that allows individuals to specify the types of medical treatment they would or would not want to receive in certain situations, such as life-sustaining treatment in the event of a terminal illness or permanent unconsciousness.
- Healthcare power of attorney: A healthcare power of attorney, also known as a healthcare proxy or durable power of attorney for healthcare, allows individuals to appoint a trusted person to make healthcare decisions on their behalf if they are unable to do so. The healthcare proxy is authorized to make decisions based on the individual’s wishes as expressed in the advance directive or, if those wishes are not known, based on what the proxy believes to be in the individual’s best interests.
- Do Not Resuscitate (DNR) order: A DNR order is a medical order that instructs healthcare providers not to attempt cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. DNR orders are typically written by a healthcare provider based on the individual’s wishes or advance directive.
Advance directives are important tools for ensuring that individuals receive the care they want and avoid treatments they do not want, even if they are unable to communicate their wishes. It is important for individuals to discuss their wishes with their healthcare providers and family members and to ensure that their advance directives are up-to-date and easily accessible in case of an emergency.
What kinds of questions are dealt with by a living will?
A living will, also known as an advance directive, addresses specific medical treatment decisions that may arise if a person becomes incapacitated and is unable to communicate their wishes. The document outlines the individual’s preferences regarding end-of-life care and other medical interventions. Common questions that are addressed by a living will include:
- Life-sustaining treatments: A living will typically addresses whether or not a person wants to receive life-sustaining treatments, such as CPR (cardiopulmonary resuscitation), mechanical ventilation, artificial nutrition and hydration (tube feeding), and dialysis, in the event of a terminal illness or irreversible coma.
- Palliative care: A living will may specify whether the individual wants to receive palliative care, which focuses on relieving pain and improving quality of life, even if it means foregoing life-prolonging treatments.
- Organ donation: Some living wills include provisions regarding organ and tissue donation, specifying whether or not the individual wishes to donate their organs and under what circumstances.
- Comfort care: A living will may address preferences for comfort care, such as pain management and emotional support, at the end of life.
- Specific medical conditions: A living will may address specific medical conditions or scenarios and provide guidance on treatment preferences for those situations.
It’s important for individuals to carefully consider their values, beliefs, and healthcare preferences when creating a living will and to discuss their wishes with their healthcare providers and family members. Living wills are legally binding documents that provide guidance to healthcare providers and family members in making decisions about medical treatment in accordance with the individual’s wishes.
How should I choose somebody for medical power of attorney?
Choosing someone to be your healthcare power of attorney, also known as a healthcare proxy, is an important decision. This person will be responsible for making medical decisions on your behalf if you become unable to do so. Here are some factors to consider when selecting a healthcare proxy:
- Trust and confidence: Choose someone you trust completely to make decisions that align with your wishes, even if they differ from their own beliefs. This person should be able to handle the responsibility and stress of making difficult medical decisions.
- Availability and proximity: Your healthcare proxy should be someone who is readily available and able to be present if needed, especially in emergencies. Consider someone who lives nearby or can easily travel to your location.
- Understanding of your wishes: Your healthcare proxy should understand your values, beliefs, and preferences regarding medical treatment. Have a thorough conversation with them about your wishes and make sure they are comfortable advocating for you.
- Communication skills: Choose someone who is a good communicator and can effectively communicate with healthcare providers and other family members. They should be able to ask questions, seek clarification, and relay information accurately.
- Legal and emotional maturity: Your healthcare proxy should be legally competent and emotionally mature to handle the responsibilities of making medical decisions on your behalf.
- Backup proxy: Consider selecting a backup healthcare proxy in case your primary proxy is unable or unwilling to fulfill their role.
- Consult with healthcare providers: Consider discussing your choice of healthcare proxy with your healthcare providers to ensure they understand the responsibilities involved and are willing to support your proxy in making decisions.
It’s important to discuss your wishes and expectations with your chosen healthcare proxy and to document your choice in a legal document, such as a healthcare power of attorney. This document should be kept in a safe place and shared with your healthcare providers and family members.