Amenorrhea: Symptoms, Causes, Treatment
What are the symptoms of amenorrhea?
Amenorrhea is the absence of menstruation, and it can be classified into two types: primary amenorrhea, when a female has not started menstruating by the age of 16, and secondary amenorrhea, when a female who has previously menstruated stops menstruating for three or more consecutive months. The symptoms of amenorrhea can vary depending on the underlying cause and whether it is primary or secondary. Common symptoms may include:
- Absence of menstrual periods: The primary symptom of amenorrhea is the absence of menstrual periods. In primary amenorrhea, this means that a female has not started menstruating by the age of 16. In secondary amenorrhea, this means that a female who has previously menstruated stops menstruating for three or more consecutive months.
- Changes in breast size or texture: Hormonal imbalances that cause amenorrhea can also affect breast development. Some females with amenorrhea may experience changes in breast size or texture.
- Headaches: Hormonal changes associated with amenorrhea can sometimes cause headaches or migraines.
- Milky discharge from the breasts: In some cases of secondary amenorrhea, a milky discharge from the breasts, known as galactorrhea, may occur due to elevated levels of prolactin, a hormone that stimulates milk production.
- Hair loss: Hormonal imbalances associated with amenorrhea can sometimes lead to hair loss or thinning.
- Excess facial hair: Some females with hormonal imbalances that cause amenorrhea may experience excess facial hair growth, known as hirsutism.
- Acne: Hormonal imbalances associated with amenorrhea can sometimes lead to acne or oily skin.
- Pelvic pain: Some females with amenorrhea may experience pelvic pain or discomfort, particularly if the underlying cause is related to conditions such as polycystic ovary syndrome (PCOS) or endometriosis.
It’s important to note that amenorrhea can have many different causes, and the symptoms can vary widely among individuals. If you are experiencing symptoms of amenorrhea, it’s important to consult with a healthcare professional for proper evaluation and diagnosis.
What are the causes of amenorrhea?
Amenorrhea can have several causes, which can vary depending on whether it is primary or secondary amenorrhea. Some common causes of amenorrhea include:
- Pregnancy: The most common cause of secondary amenorrhea is pregnancy. If a female of reproductive age stops menstruating for three or more consecutive months, pregnancy should be ruled out as a possible cause.
- Hormonal imbalances: Hormonal imbalances, such as those caused by polycystic ovary syndrome (PCOS), thyroid disorders, or disorders of the pituitary or adrenal glands, can disrupt the menstrual cycle and lead to amenorrhea.
- Stress: Physical or emotional stress can disrupt the normal function of the hypothalamus, a part of the brain that regulates the menstrual cycle, leading to amenorrhea.
- Low body weight: Excessive exercise, eating disorders, or rapid weight loss can lead to low body weight, which can disrupt the production of hormones necessary for menstruation and lead to amenorrhea.
- Menopause: Menopause is a natural process that occurs in females typically around the age of 45 to 55, leading to the cessation of menstruation.
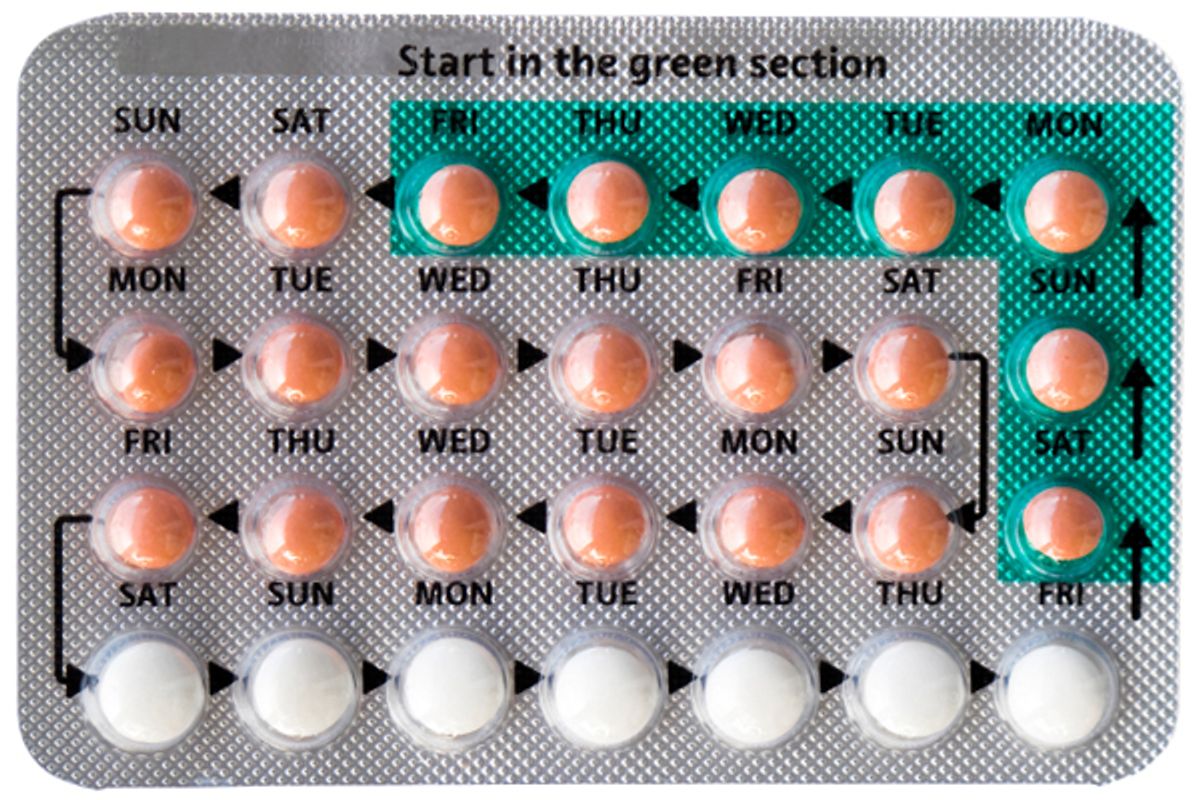
- Medications: Certain medications, such as hormonal contraceptives, antipsychotics, chemotherapy drugs, or some medications used to treat hypertension, can disrupt the menstrual cycle and lead to amenorrhea.
- Structural problems: Structural problems in the reproductive organs, such as congenital abnormalities or scarring from surgery or infection, can interfere with menstruation and lead to amenorrhea.
- Chronic conditions: Chronic conditions such as diabetes, celiac disease, or autoimmune disorders can affect hormone levels and lead to amenorrhea.
- Genetic factors: In some cases, genetic factors may play a role in amenorrhea, particularly in cases of primary amenorrhea where there is a delay in the onset of menstruation.
It’s important to note that the underlying cause of amenorrhea can vary widely among individuals, and in some cases, the cause may not be immediately apparent. If you are experiencing amenorrhea, it’s important to consult with a healthcare professional for proper evaluation and diagnosis.
What is the treatment for amenorrhea?
The treatment for amenorrhea depends on the underlying cause of the condition. In some cases, no treatment may be necessary, especially if the amenorrhea is due to factors such as pregnancy, menopause, or temporary hormonal changes. However, if treatment is required, it will be tailored to address the specific cause of the amenorrhea. Some common treatment approaches for amenorrhea include:
- Hormone therapy: Hormone therapy, such as birth control pills or hormone replacement therapy, may be used to regulate the menstrual cycle and restore normal menstruation in cases where hormonal imbalances are the cause of amenorrhea.
- Lifestyle changes: Making lifestyle changes such as reducing stress, maintaining a healthy weight, and moderating exercise levels can help restore normal menstruation in cases where these factors are contributing to amenorrhea.
- Treatment of underlying conditions: If amenorrhea is caused by an underlying condition such as polycystic ovary syndrome (PCOS), thyroid disorders, or pituitary or adrenal gland disorders, treatment of these conditions may help restore normal menstruation.
- Medication adjustments: If amenorrhea is caused by medications such as antipsychotics or chemotherapy drugs, adjusting or discontinuing these medications may help restore normal menstruation.
- Surgery: In some cases, surgical intervention may be necessary to correct structural problems in the reproductive organs that are causing amenorrhea.
- Fertility treatment: In cases where amenorrhea is associated with infertility, fertility treatments such as ovulation induction or in vitro fertilization (IVF) may be considered.
The specific treatment approach for amenorrhea will depend on the underlying cause of the condition and should be determined by a healthcare professional. It’s important for individuals experiencing amenorrhea to consult with a healthcare provider for proper evaluation and diagnosis.
TL;DR: Amenorrhea Summary
Amenorrhea is a medical term used to describe the absence of menstruation, the monthly shedding of the uterine lining that normally occurs in women of reproductive age. There are two main types of amenorrhea:
- Primary amenorrhea: Primary amenorrhea refers to the absence of menstruation by the age of 16, without the onset of puberty, or by the age of 14 with no secondary sexual characteristics. It can be caused by factors such as hormonal imbalances, anatomical abnormalities of the reproductive organs, genetic conditions, or chronic illnesses.
- Secondary amenorrhea: Secondary amenorrhea occurs when a woman who has had regular menstrual cycles stops menstruating for three consecutive months or more. It can be caused by factors such as pregnancy, breastfeeding, hormonal changes (such as polycystic ovary syndrome or thyroid disorders), excessive exercise, stress, eating disorders, or certain medications.
Symptoms of amenorrhea may vary depending on the underlying cause but can include:
- Absence of menstrual bleeding
- Changes in weight or appetite
- Hair loss
- Acne
- Headaches
- Vision changes
- Milky discharge from the breasts
Diagnosis and treatment of amenorrhea depend on the underlying cause. A healthcare provider may perform a physical examination, blood tests to check hormone levels, imaging studies to evaluate the reproductive organs, and other tests as needed. Treatment may involve addressing the underlying cause of the amenorrhea, such as hormone therapy, lifestyle modifications, or medication.
It is essential for individuals experiencing amenorrhea to seek medical evaluation to determine the cause and receive appropriate treatment. Untreated amenorrhea can lead to long-term complications such as infertility, bone loss (osteoporosis), and an increased risk of certain health conditions. With proper diagnosis and treatment, many cases of amenorrhea can be effectively managed and menstrual cycles restored to normal.