Rheumatoid Arthritis: Symptoms, Causes, Treatment
What are the symptoms of rheumatoid arthritis?
Rheumatoid arthritis (RA) is an autoimmune disorder that primarily affects the joints, causing inflammation, pain, stiffness, and swelling. The symptoms of RA can vary widely from person to person, but some common symptoms include:
- Joint pain: RA often causes pain in the joints, typically affecting the same joints on both sides of the body (symmetrical joint involvement). The pain is often worse in the morning or after periods of inactivity.
- Joint stiffness: Stiffness in the joints, especially in the morning or after periods of inactivity, is a common symptom of RA. Stiffness may last for a few hours or throughout the day.
- Swelling: RA can cause swelling and tenderness in the joints, making them appear red and warm to the touch.
- Fatigue: Many people with RA experience fatigue, which can be debilitating and impact daily activities.
- Joint deformities: Over time, RA can cause joint deformities, especially in the hands and feet. This can lead to difficulty with fine motor skills and grip strength.
- Loss of joint function: As RA progresses, it can lead to a loss of joint function and mobility, making it difficult to perform daily tasks.
- Other symptoms: RA can also cause other symptoms, such as fever, weight loss, and a general feeling of malaise.
It’s important to note that the symptoms of RA can vary in severity and may come and go over time, with periods of flare-ups and remission. If you experience persistent joint pain, stiffness, or swelling, it’s important to see a healthcare provider for an accurate diagnosis and appropriate treatment. Early diagnosis and treatment can help manage symptoms and slow the progression of the disease.
What are the causes of rheumatoid arthritis?
Rheumatoid arthritis (RA) is an autoimmune disorder, which means that the immune system mistakenly attacks the body’s own tissues, primarily affecting the joints. The exact cause of RA is not known, but it is believed to involve a combination of genetic, environmental, and hormonal factors.
- Genetics: There is evidence to suggest that genetics plays a role in the development of RA. People with a family history of RA are at an increased risk of developing the condition.
- Immune system dysfunction: In RA, the immune system mistakenly attacks the synovium, the lining of the membranes that surround the joints. This results in inflammation and thickening of the synovium, which can eventually lead to joint damage.
- Environmental factors: Certain environmental factors, such as smoking, exposure to pollutants, and infections, may contribute to the development of RA in people who are genetically predisposed to the condition.
- Hormones: Hormonal factors, particularly in women, may play a role in the development of RA. The disease is more common in women than men, and hormonal changes, such as those that occur during pregnancy or menopause, can affect the immune system and potentially contribute to the development of RA.
- Other factors: Other factors, such as obesity, may also play a role in the development of RA. Obesity is associated with an increased risk of RA and may contribute to disease progression.
It’s important to note that while these factors may increase the risk of developing RA, they do not guarantee that a person will develop the condition. The development of RA is likely to be influenced by a combination of genetic, environmental, and hormonal factors.
What is the treatment for rheumatoid arthritis?
The treatment for rheumatoid arthritis (RA) aims to reduce inflammation, relieve symptoms, prevent joint damage, and improve overall quality of life. Treatment typically involves a combination of medications, lifestyle changes, and other therapies. The specific treatment plan for RA may vary depending on the severity of the disease, the individual’s symptoms, and their response to treatment. Some common treatments for RA include:
- Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen or naproxen, can help reduce pain and inflammation.
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs, such as methotrexate, hydroxychloroquine, or sulfasalazine, are used to slow the progression of RA and prevent joint damage.
- Biologic agents: Biologic agents, such as tumor necrosis factor (TNF) inhibitors, interleukin-6 (IL-6) inhibitors, or other biologic therapies, are used to target specific components of the immune system involved in RA.
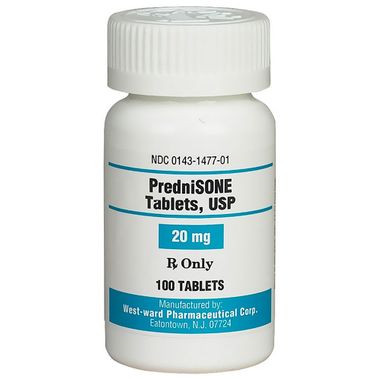
- Corticosteroids: Corticosteroids, such as prednisone, may be used to reduce inflammation and suppress the immune system during flare-ups.
- Lifestyle changes:
- Exercise: Regular exercise, including strength training and low-impact aerobic exercises, can help improve joint function and reduce pain and stiffness.
- Healthy diet: A balanced diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids can help reduce inflammation and improve overall health.
- Rest: Adequate rest is important to reduce joint pain and fatigue associated with RA.
- Physical therapy: Physical therapy can help improve joint function, flexibility, and strength through targeted exercises and techniques.
- Occupational therapy: Occupational therapy can help people with RA learn new ways to perform daily tasks to reduce strain on their joints.
- Surgery: In severe cases of RA where joint damage is extensive, surgery may be necessary to repair or replace damaged joints.
- Alternative therapies: Some people with RA find relief from symptoms through alternative therapies, such as acupuncture, massage, or dietary supplements. It’s important to talk to a healthcare provider before trying any alternative therapies to ensure they are safe and effective.
It’s important for people with RA to work closely with a healthcare provider to develop a treatment plan that meets their individual needs. Treatment may need to be adjusted over time based on the person’s symptoms and response to therapy. Early diagnosis and treatment of RA can help manage symptoms and improve long-term outcomes.
TL; DR: Rheumatoid Arthritis Summary
Rheumatoid Arthritis (RA) is a chronic autoimmune disease that primarily affects the joints, causing inflammation, pain, stiffness, and swelling. It’s like your body’s defense system has decided your joints are the enemy and starts attacking them. This can lead to damage of the joint tissue, cartilage, and even the bone itself. It’s not just a pain in the joints, though; RA can also affect other parts of the body like the lungs, heart, and eyes. The onset of RA is highest among adults in their 50s, but it can hit at any age. There’s no cure for RA yet, but there are treatments to manage the symptoms and slow down the disease progression. So, if you’re feeling a bit stiff and sore, it might be time to chat with your healthcare provider.