Balo’s Disease: Symptoms, Causes, Treatment
What are the symptoms of Balo’s disease?
Balo’s concentric sclerosis, also known as Balo’s disease, is a rare and aggressive form of multiple sclerosis (MS). The main symptoms of Balo’s disease are related to the formation of concentric lesions or rings of demyelination in the brain and spinal cord. These symptoms can include:
- Neurological deficits: Depending on the location of the lesions, patients may experience various neurological deficits, such as:
- Weakness or paralysis in the limbs
- Loss of sensation or numbness
- Vision problems or vision loss
- Speech difficulties
- Cognitive impairment
- Balance and coordination issues
- Seizures: Some patients with Balo’s disease may experience seizures due to the lesions in the brain.
- Headaches: Severe headaches can occur as a result of the inflammation and lesions in the brain.
- Fatigue: Overwhelming fatigue is a common symptom, especially during active disease flare-ups.
- Bladder and bowel problems: Lesions in the spinal cord can lead to bladder and bowel dysfunction.
- Pain: Neuropathic pain or discomfort can occur due to the demyelination and nerve damage.
- Mental and emotional changes: Patients may experience changes in mood, depression, or other psychological symptoms due to the effects of the disease on the brain.
The symptoms of Balo’s disease can vary widely depending on the location, size, and number of lesions in the central nervous system. The onset of symptoms is typically rapid and progressive, often leading to significant disability within weeks or months if left untreated.
It’s important to note that Balo’s disease is an extremely rare condition, and its symptoms can overlap with other demyelinating disorders like multiple sclerosis or acute disseminated encephalomyelitis (ADEM). Prompt diagnosis and treatment with aggressive immunosuppressive therapies are crucial to manage the disease and prevent permanent neurological damage.
What are the causes of Balo’s disease?
The exact causes of Balo’s concentric sclerosis, or Balo’s disease, are not well understood. However, it is believed to have an autoimmune component, similar to other demyelinating diseases like multiple sclerosis (MS). Some potential causes and factors that may contribute to the development of Balo’s disease include:
- Autoimmune reaction: Balo’s disease is thought to be an autoimmune disorder, where the body’s immune system mistakenly attacks and destroys the myelin sheath that surrounds and protects nerve fibers in the brain and spinal cord.
- Genetic factors: There may be a genetic predisposition or certain genetic variations that increase an individual’s susceptibility to developing autoimmune demyelinating disorders like Balo’s disease.
- Environmental triggers: Certain environmental factors, such as viral infections, exposure to toxins, or other environmental triggers, may potentially initiate or exacerbate the autoimmune response leading to Balo’s disease in genetically predisposed individuals.
- Molecular mimicry: It is hypothesized that the immune system may mistake certain components of the myelin sheath for foreign antigens, leading to an autoimmune attack due to molecular mimicry with pathogens like viruses or bacteria.
- Disruption of the blood-brain barrier: Some researchers believe that a disruption or increased permeability of the blood-brain barrier, which normally protects the brain from harmful substances, may play a role in the development of Balo’s disease by allowing immune cells or antibodies to enter the central nervous system.
- Vitamin D deficiency: Low levels of vitamin D have been associated with an increased risk of autoimmune diseases, including demyelinating disorders like Balo’s disease.
It’s important to note that Balo’s disease is an extremely rare condition, and its exact causes are still not fully understood. More research is needed to better understand the underlying mechanisms and potential triggers that lead to the development of this aggressive form of demyelinating disease.
What is the treatment for Balo’s disease?
The treatment for Balo’s concentric sclerosis, or Balo’s disease, typically involves aggressive immunosuppressive and immunomodulatory therapies aimed at reducing the autoimmune response and preventing further demyelination and neurological damage. Here are some of the common treatment approaches:
- Corticosteroids: High-dose intravenous corticosteroids, such as methylprednisolone, are often used as the initial treatment to reduce inflammation and suppress the immune system’s attack on the myelin sheath.
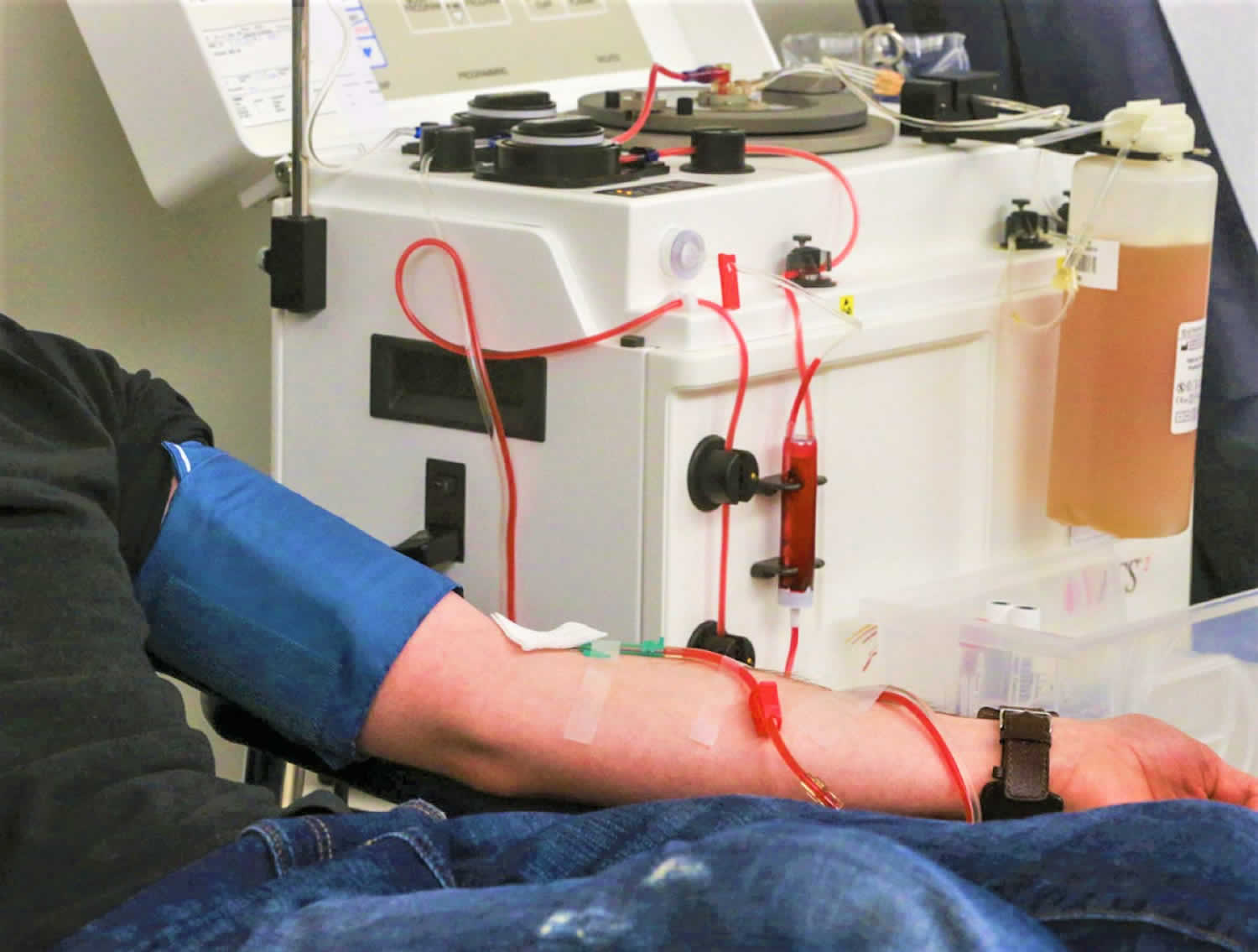
- Plasma exchange (plasmapheresis): This procedure involves removing the patient’s plasma (the liquid portion of blood) and replacing it with new plasma or a plasma substitute. It helps remove harmful antibodies or other substances that may be contributing to the autoimmune process.
- Intravenous immunoglobulin (IVIG): IVIG therapy involves administering purified antibodies intravenously, which can help modulate the immune system’s response and reduce inflammation.
- Immunosuppressive medications: Various immunosuppressive drugs, such as cyclophosphamide, azathioprine, methotrexate, or rituximab, may be prescribed to suppress the overactive immune system and prevent further demyelination.
- Monoclonal antibodies: Medications like natalizumab or alemtuzumab, which are monoclonal antibodies that target specific components of the immune system, may be used in some cases to help control the autoimmune response.
- Stem cell transplantation: In severe cases or cases that do not respond to other treatments, autologous hematopoietic stem cell transplantation (HSCT) may be considered. This procedure involves using the patient’s own stem cells to rebuild their immune system after intensive chemotherapy or radiation therapy.
- Supportive care: In addition to immunotherapy, supportive care measures such as physical therapy, occupational therapy, and management of symptoms like seizures, pain, and bladder or bowel dysfunction may be necessary.
It’s important to note that Balo’s disease is an extremely rare and aggressive condition, and the treatment approach is often individualized based on the patient’s specific circumstances and response to therapy. Close monitoring and frequent follow-up by your healthcare provider are essential to assess the effectiveness of the treatment and make any necessary adjustments.