Amyloidosis: Symptoms, Causes, Treatment
What are the symptoms of amyloidosis?
Amyloidosis is a rare condition caused by the buildup of abnormal proteins called amyloids in various organs and tissues in the body. The symptoms of amyloidosis can vary depending on the organs affected and the extent of amyloid deposition. Some common symptoms of amyloidosis may include:
- Fatigue: Feeling tired or weak, often due to anemia or other effects of amyloidosis on organ function.
- Swelling: Swelling in the ankles, legs, or other parts of the body due to fluid retention.
- Shortness of breath: Difficulty breathing, especially with exertion, due to heart or lung involvement.
- Numbness or tingling: Sensations of numbness, tingling, or pain in the hands or feet, often due to nerve damage.
- Weight loss: Unintentional weight loss, often due to loss of appetite or effects on organ function.
- Enlarged tongue: The tongue may become enlarged and stiff, making it difficult to speak or eat.
- Skin changes: Changes in the skin, such as easy bruising or a waxy appearance.
- Heart problems: Amyloidosis can affect the heart, leading to symptoms such as irregular heart rhythms, shortness of breath, and swelling of the legs and abdomen.
- Kidney problems: Amyloidosis can affect the kidneys, leading to symptoms such as swelling, protein in the urine, and decreased kidney function.
- Liver problems: Amyloidosis can affect the liver, leading to symptoms such as an enlarged liver, fatigue, and jaundice (yellowing of the skin and eyes).
- Gastrointestinal problems: Amyloidosis can affect the gastrointestinal tract, leading to symptoms such as diarrhea, constipation, and difficulty swallowing.
It’s important to note that the symptoms of amyloidosis can vary widely among affected individuals, and some individuals may have no symptoms at all, especially in the early stages of the condition. If you have symptoms suggestive of amyloidosis, it’s important to see your healthcare provider for an accurate diagnosis and appropriate management.
What are the causes of amyloidosis?
Amyloidosis is caused by the abnormal accumulation of proteins called amyloids in various tissues and organs of the body. These amyloid proteins are typically produced in the bone marrow and are normally broken down and cleared from the body. However, in amyloidosis, the proteins are not broken down properly and instead accumulate in tissues and organs, disrupting their normal function.
There are several types of amyloidosis, each with its own underlying cause:
- Primary amyloidosis (AL): This type of amyloidosis is caused by the abnormal production of immunoglobulin light chains, which are proteins produced by abnormal plasma cells in the bone marrow. Primary amyloidosis is typically associated with plasma cell disorders such as multiple myeloma.
- Secondary amyloidosis (AA): This type of amyloidosis is caused by the buildup of a protein called serum amyloid A (SAA), which is produced in response to inflammation or chronic infection. Secondary amyloidosis is often associated with chronic inflammatory diseases such as rheumatoid arthritis or inflammatory bowel disease (Crohn’s disease or ulcerative colitis).
- Hereditary amyloidosis: This type of amyloidosis is caused by genetic mutations that affect the production or structure of certain proteins, leading to their abnormal accumulation in tissues and organs. Hereditary amyloidosis can affect different organs depending on the specific genetic mutation involved.
- Senile amyloidosis: This type of amyloidosis occurs with aging and is caused by the buildup of a protein called transthyretin (TTR) in the heart and other tissues. Senile amyloidosis is more common in older individuals and is typically not associated with a genetic mutation.
- Dialysis-related amyloidosis: This type of amyloidosis occurs in individuals who have been on long-term dialysis treatment for kidney failure. The buildup of beta-2 microglobulin, a protein that is not effectively removed by dialysis, can lead to amyloidosis.
The exact cause of amyloidosis can vary depending on the type of amyloidosis. In many cases, the underlying cause of amyloidosis is not known, and the condition is referred to as idiopathic amyloidosis.
What is the treatment for amyloidosis?
The treatment for amyloidosis depends on the type of amyloidosis, the organs affected, and the severity of the condition. Treatment may include:
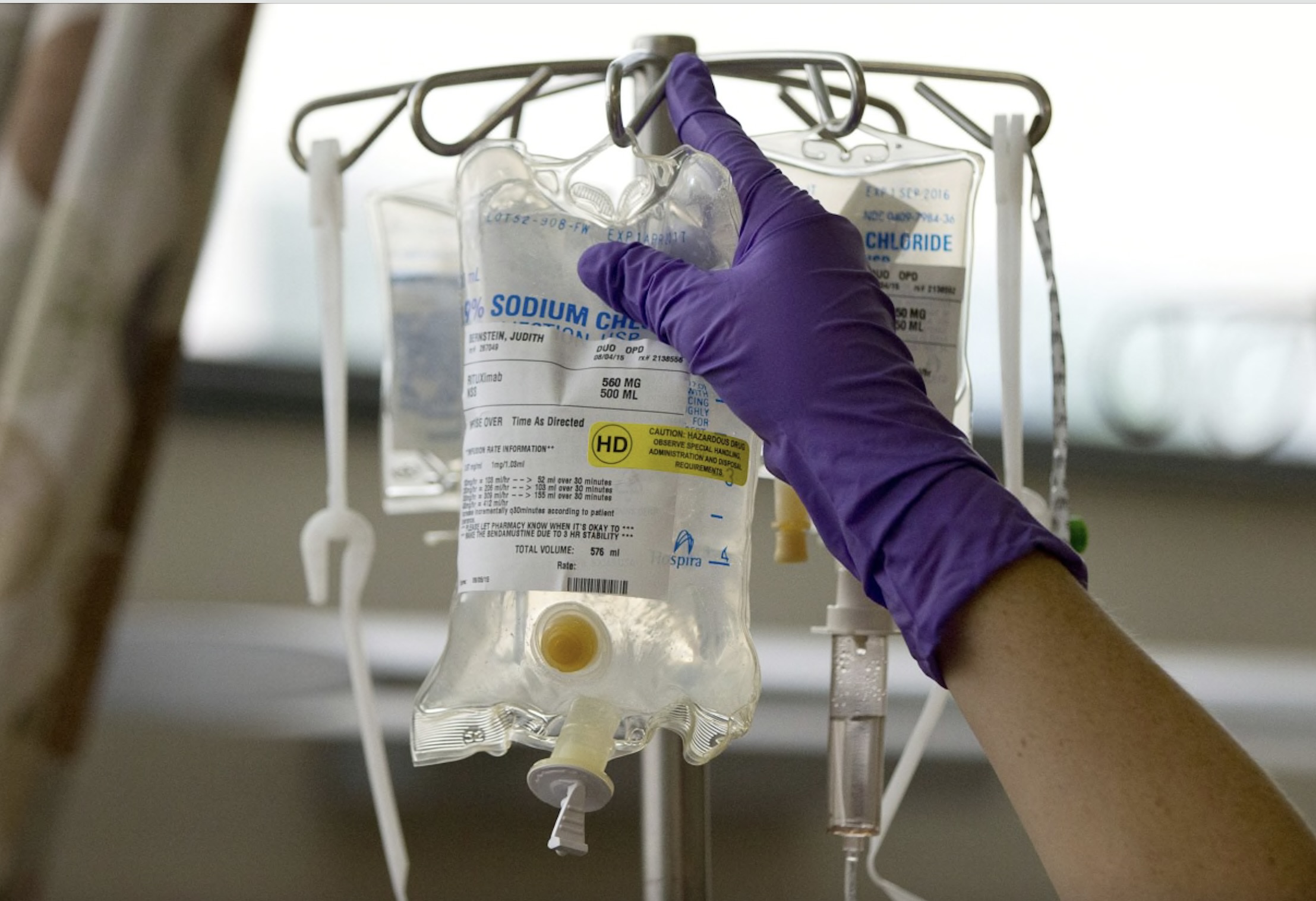
- Chemotherapy: For primary (AL) amyloidosis, chemotherapy may be used to reduce the production of abnormal proteins by plasma cells in the bone marrow. This can help slow the progression of the disease and reduce symptoms.
- Stem cell transplant: In some cases of primary (AL) amyloidosis, a stem cell transplant may be recommended to replace diseased bone marrow with healthy stem cells that can produce normal blood cells and proteins.
- Targeted therapy: Newer targeted therapies, such as proteasome inhibitors and immunomodulatory drugs, may be used to treat primary (AL) amyloidosis by targeting the abnormal plasma cells.
- Anti-inflammatory medications: For secondary (AA) amyloidosis, medications that reduce inflammation, such as corticosteroids or other immunosuppressive drugs, may be used to reduce the production of the protein that forms amyloids.
- Liver transplant: In hereditary amyloidosis (such as transthyretin amyloidosis), a liver transplant may be considered to replace the liver, which is the main source of the abnormal protein, with a healthy liver that does not produce the abnormal protein.
- Symptom management: Treatment may also focus on managing symptoms and complications of amyloidosis, such as heart failure, kidney failure, and neuropathy. This may include medications to control blood pressure, fluid retention, and heart rhythm, as well as supportive care such as physical therapy and occupational therapy.
- Clinical trials: Participation in clinical trials of new treatments for amyloidosis may be an option for some patients, particularly those with advanced or refractory disease.
It’s important for individuals with amyloidosis to work closely with a healthcare team experienced in managing the condition to develop a personalized treatment plan. Treatment may need to be adjusted over time based on the individual’s response to therapy and the progression of the disease.
Amyloidosis Summary
Amyloidosis is a rare disease that occurs when abnormal protein deposits called amyloids build up in tissues and organs, interfering with their normal functioning. There are several types of amyloidosis, and the symptoms and complications can vary depending on the specific type and the organs affected.
Some common types of amyloidosis include:
- AL amyloidosis (primary systemic amyloidosis): This type of amyloidosis is caused by the abnormal buildup of immunoglobulin light chain proteins in tissues and organs. It most commonly affects the heart, kidneys, liver, and nerves, leading to symptoms such as fatigue, shortness of breath, swelling, heart problems, kidney dysfunction, and neurological issues.
- AA amyloidosis (secondary amyloidosis): AA amyloidosis occurs when a protein called serum amyloid A (SAA) builds up in tissues and organs in response to chronic inflammation or infections. It can affect the kidneys, liver, spleen, and gastrointestinal tract, and symptoms may include swelling, fatigue, weight loss, and kidney dysfunction.
- Hereditary amyloidosis: This type of amyloidosis is inherited and caused by mutations in genes that produce specific proteins prone to forming amyloid deposits. It can affect the heart, nerves, kidneys, and other organs, leading to symptoms such as heart failure, neuropathy, kidney dysfunction, and gastrointestinal issues.
Treatment for amyloidosis depends on the type and severity of the disease, as well as the organs affected. It may include medications to target the underlying cause, manage symptoms, and reduce the production of the abnormal proteins. In some cases, treatments such as chemotherapy, stem cell transplants, or organ transplants may be necessary.
It is important for individuals with amyloidosis to work closely with a healthcare team, including specialists in hematology, nephrology, cardiology, and other relevant fields, to develop a personalized treatment plan that addresses their specific needs and symptoms. Early diagnosis and treatment are crucial in managing amyloidosis and minimizing its impact on overall health and quality of life.