Bacterial Vaginosis: Symptoms, Causes & Treatment
What are the symptoms of bacterial vaginosis?
Bacterial vaginosis (BV) is a type of vaginal inflammation caused by an overgrowth of certain bacteria. Here are the common symptoms of bacterial vaginosis:
- Abnormal vaginal discharge: The most common symptom is a thin, grayish-white or yellow discharge that may have a fishy odor, especially after intercourse or during menstruation.
- Vaginal odor: Many women with BV experience a strong, fishy odor, especially after sexual intercourse or during menstruation.
- Vaginal itching: Some women may experience vaginal itching or irritation, although this is not as common as the abnormal discharge or odor.
- Burning sensation: In some cases, bacterial vaginosis can cause a burning sensation when urinating or during intercourse.
It’s important to note that some women with bacterial vaginosis may not experience any noticeable symptoms at all. However, even without symptoms, BV can increase the risk of other complications, such as:
- Preterm delivery or low birth weight in pregnant women
- Increased risk of contracting sexually transmitted infections (STIs) like HIV, chlamydia, and gonorrhea
- Post-surgical infections (e.g., after hysterectomy or abortion)
Bacterial vaginosis is caused by an imbalance in the vaginal microbiome, where there is an overgrowth of certain bacteria, such as Gardnerella vaginalis, and a decrease in beneficial lactobacilli bacteria.
If you experience any abnormal vaginal discharge, odor, or other symptoms, it’s important to seek medical attention from a healthcare provider for proper diagnosis and treatment. BV is generally treated with antibiotics or vaginal gels to restore the balance of vaginal bacteria.
What are the causes of bacterial vaginosis?
Bacterial vaginosis (BV) is caused by an overgrowth of certain bacteria in the vagina, leading to an imbalance in the normal vaginal flora. The exact causes are not fully understood, but several factors are thought to contribute to the development of BV:
- Douching: Frequent douching can disrupt the natural balance of bacteria in the vagina and increase the risk of BV.
- New or multiple sexual partners: Having a new sexual partner or multiple sexual partners can introduce new bacteria into the vagina, potentially leading to an overgrowth.
- Unprotected sex: Engaging in unprotected sex can increase the risk of contracting BV, as well as other sexually transmitted infections (STIs).
- Hormonal changes: Fluctuations in hormones during menstruation, pregnancy, or hormonal contraceptive use can alter the vaginal environment and make it more susceptible to bacterial overgrowth.
- Intrauterine device (IUD) use: The use of an IUD for contraception has been associated with a slightly increased risk of BV, possibly due to the presence of a foreign body in the vagina.
- Smoking: Smoking can decrease the levels of beneficial lactobacilli bacteria in the vagina, potentially allowing other bacteria to overgrow.
- Antibiotics: The use of certain antibiotics can disrupt the natural vaginal flora, creating an environment conducive to BV.
- Genetic factors: Some women may have a genetic predisposition that makes them more susceptible to developing BV.
It’s important to note that BV is not considered a sexually transmitted infection (STI), although it is more common in sexually active women. BV is generally not considered a serious condition, but it can increase the risk of other complications, such as preterm birth or acquiring STIs. If left untreated, BV can lead to recurrent infections or other complications.
What is the treatment for bacterial vaginosis?
The treatment for bacterial vaginosis (BV) typically involves antibiotic therapy to help restore the balance of bacteria in the vagina. The recommended treatments include:
- Oral antibiotics:
- Metronidazole (Flagyl) is the most commonly prescribed oral antibiotic for BV. It is taken twice daily for 5-7 days.
- Clindamycin is an alternative oral antibiotic that can be used if metronidazole is not tolerated or is ineffective.
- Vaginal antibiotics:
- Metronidazole gel or vaginal suppositories can be used for 5 days as an alternative to oral antibiotics.
- Clindamycin vaginal cream is another option for vaginal application for 7 days.
- Tinidazole (Tindamax):
- This is a single-dose oral antibiotic that can be used as an alternative to the multi-dose regimens.
In addition to antibiotic treatment, some additional recommendations may include:
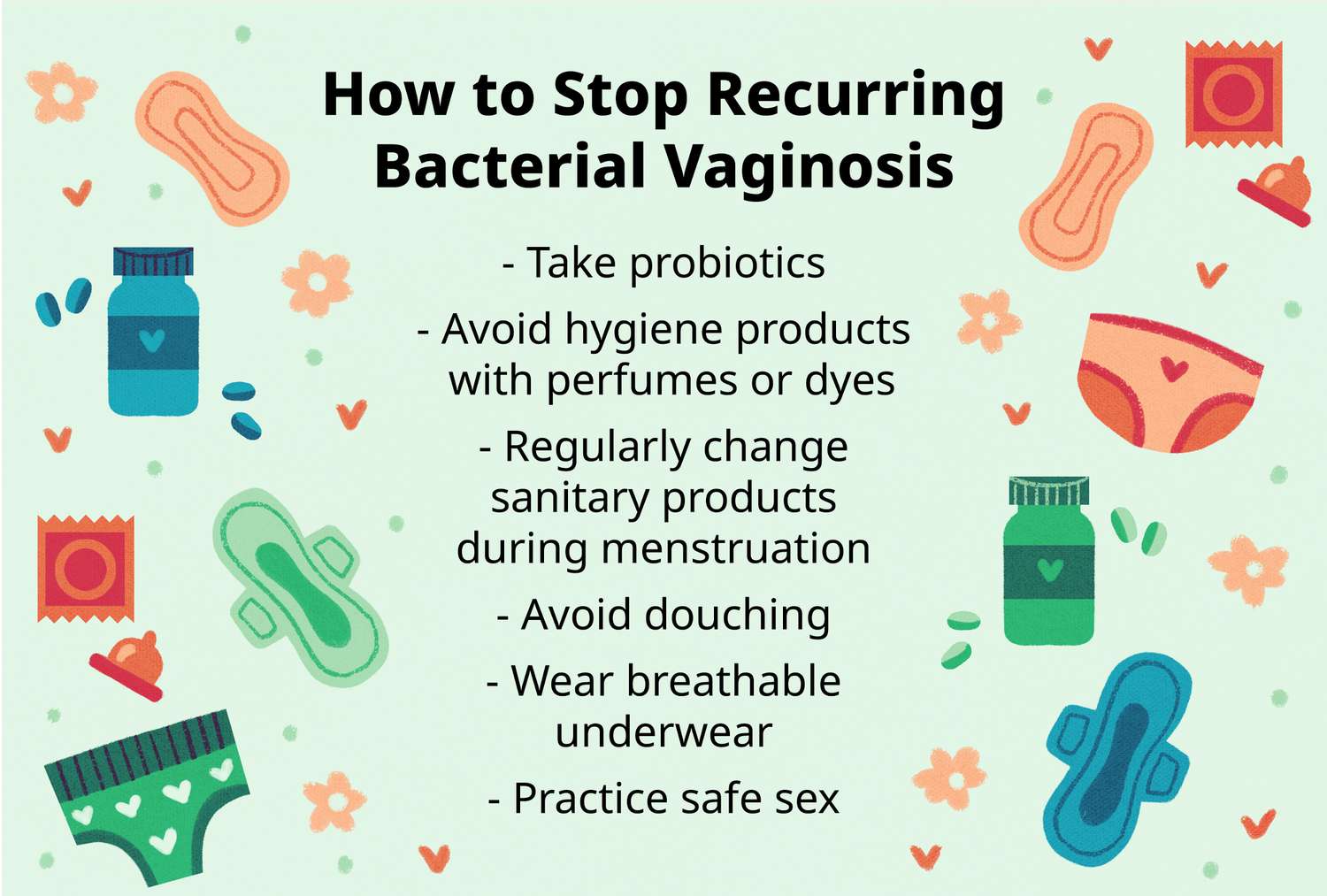
- Avoid douching: Douching can disrupt the vaginal flora and make BV more likely to recur.
- Use condoms: Using condoms during sexual activity can help prevent the transmission of BV-associated bacteria between partners.
- Treat sexual partners: In some cases, healthcare providers may recommend treating male sexual partners to prevent the transmission of BV between partners.
- Avoid unnecessary antibiotic use: Antibiotics can disrupt the vaginal flora, so they should only be taken when necessary.
It’s important to complete the full course of antibiotics as prescribed, even if symptoms improve, to ensure the infection is fully cleared. In some cases, BV may recur, and additional treatment may be necessary.
If symptoms persist or recur after treatment, it is recommended to consult a healthcare provider for further evaluation and management.