Behcet’s Syndrome: Symptoms, Causes and Treatment
What are the symptoms of Behcet’s syndrome?
Behcet’s syndrome is a rare, chronic inflammatory disorder that can involve multiple organ systems. The symptoms of Behcet’s syndrome can vary widely among individuals, but the most common symptoms include:
- Recurrent oral ulcers: One of the most common and earliest symptoms of Behcet’s syndrome is the development of painful mouth sores or ulcers that come and go. These ulcers can occur on the tongue, inner cheeks, and lips.
- Genital ulcers: Many people with Behcet’s syndrome experience recurrent, painful ulcers or sores on the genitals, which can occur on the scrotum or penis in men and the vulva in women.
- Eye inflammation (uveitis): Eye inflammation, particularly uveitis (inflammation of the uvea, the middle layer of the eye), is a common and serious complication of Behcet’s syndrome. If left untreated, it can lead to vision loss or blindness.
- Skin lesions: People with Behcet’s syndrome may develop various skin lesions, including acne-like lesions, erythema nodosum (tender, red nodules), and lesions that resemble pyoderma gangrenosum (painful, ulcerating lesions).
- Joint pain and swelling: Arthritis, particularly in the knees, ankles, wrists, and elbows, is a common symptom of Behcet’s syndrome.
- Gastrointestinal problems: Some individuals with Behcet’s syndrome may experience abdominal pain, diarrhea, or other gastrointestinal issues due to inflammation in the digestive tract.
- Neurological problems: In some cases, Behcet’s syndrome can affect the central nervous system, leading to symptoms such as headaches, fever, impaired coordination, and changes in personality or behavior.
- Vascular involvement: Behcet’s syndrome can also cause inflammation in blood vessels (vasculitis), which can lead to complications such as deep vein thrombosis, aneurysms, or even stroke.
The symptoms of Behcet’s syndrome can come and go in unpredictable patterns, with periods of remission and flare-ups. The severity of the condition can vary greatly, ranging from mild to potentially life-threatening complications.
Prompt diagnosis and appropriate treatment by your healthcare provider, which often involves immunosuppressive medications and other therapies, are crucial for managing the symptoms and preventing long-term complications of Behcet’s syndrome.
What are the causes of Behcet’s syndrome?
The exact cause of Behcet’s syndrome is not fully understood, but it is believed to involve a combination of genetic and environmental factors that trigger an abnormal immune system response. Here are some of the potential causes and risk factors associated with Behcet’s syndrome:
- Genetic factors: There appears to be a genetic predisposition to developing Behcet’s syndrome. The disorder is more common in certain ethnic groups, such as those from the Mediterranean region, Middle East, and East Asia, suggesting a genetic link. Specific genes, including those related to the immune system, have been associated with an increased risk.
- Environmental triggers: While not the direct cause, certain environmental factors are thought to trigger the abnormal immune response in genetically predisposed individuals. These triggers may include:
- Bacterial or viral infections
- Exposure to environmental toxins or chemicals
- Trauma or injury
- Stress
- Autoimmune response: Behcet’s syndrome is considered an autoimmune disorder, where the immune system mistakenly attacks the body’s own tissues, leading to inflammation and the characteristic symptoms.
- Dysregulated immune system: There is evidence of abnormalities in various components of the immune system in people with Behcet’s syndrome, including increased levels of certain inflammatory molecules (cytokines) and immune cell dysfunction.
- Hormonal factors: The condition is more common in adults between the ages of 20 and 40, suggesting a potential role of hormones in the development or triggering of the disease.
- Environmental factors: Certain environmental factors, such as smoking, have been associated with an increased risk of developing Behcet’s syndrome or more severe symptoms.
It is important to note that Behcet’s syndrome is not contagious and cannot be transmitted from one person to another. The exact interplay between genetic and environmental factors in triggering the disease is still being researched, and the underlying mechanisms are not fully understood.
While the causes are not entirely clear, identifying potential risk factors and understanding the immune system’s role in the development of Behcet’s syndrome can help in developing more effective treatments and management strategies for this complex disorder.
What treatments are there for Behcet’s syndrome?
There is no cure for Behcet’s syndrome, but several treatments are available to manage the symptoms and prevent complications. The treatment approach is typically tailored to each individual’s specific symptoms and the severity of the condition. The main treatment options for Behcet’s syndrome include:
- Topical treatments: For mouth and genital ulcers, topical corticosteroids, analgesics, or other topical medications may be prescribed to reduce inflammation and pain.
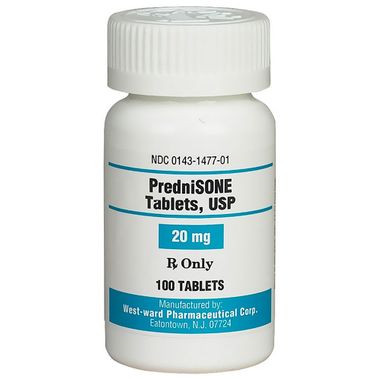
- Corticosteroids: Oral or intravenous corticosteroids, such as prednisone, are often used to control inflammation and suppress the immune system during flare-ups or severe symptoms.
- Immunosuppressive medications: Drugs that suppress the overactive immune system are commonly used to manage Behcet’s syndrome, including:
- Disease-modifying antirheumatic drugs (DMARDs) like azathioprine, methotrexate, or cyclosporine
- Biologic agents like anti-tumor necrosis factor (TNF) drugs (e.g., infliximab, adalimumab)
- Newer targeted therapies like apremilast or canakinumab
- Eye drops and medications: For eye inflammation (uveitis), corticosteroid eye drops, pupil dilators, and other medications may be used to reduce inflammation and prevent vision loss.
- Pain management: Over-the-counter or prescription pain medications may be used to alleviate joint pain, headaches, or other types of pain associated with Behcet’s syndrome.
- Surgery: In some cases, surgery may be necessary to treat complications like aneurysms, intestinal perforations, or severe eye involvement.
- Supportive care: Depending on the symptoms and complications, additional supportive care may be needed, such as physical therapy, occupational therapy, or counseling for mental health support.
- Lifestyle modifications: Certain lifestyle changes, such as quitting smoking, managing stress, and maintaining a healthy diet, may help reduce inflammation and improve overall health.
The treatment plan for Behcet’s syndrome often involves a combination of medications and supportive care measures, with the goal of controlling inflammation, managing symptoms, and preventing long-term complications. Regular monitoring and follow-up with a healthcare team, including rheumatologists, ophthalmologists, and other specialists, is crucial for effective management of this complex condition.