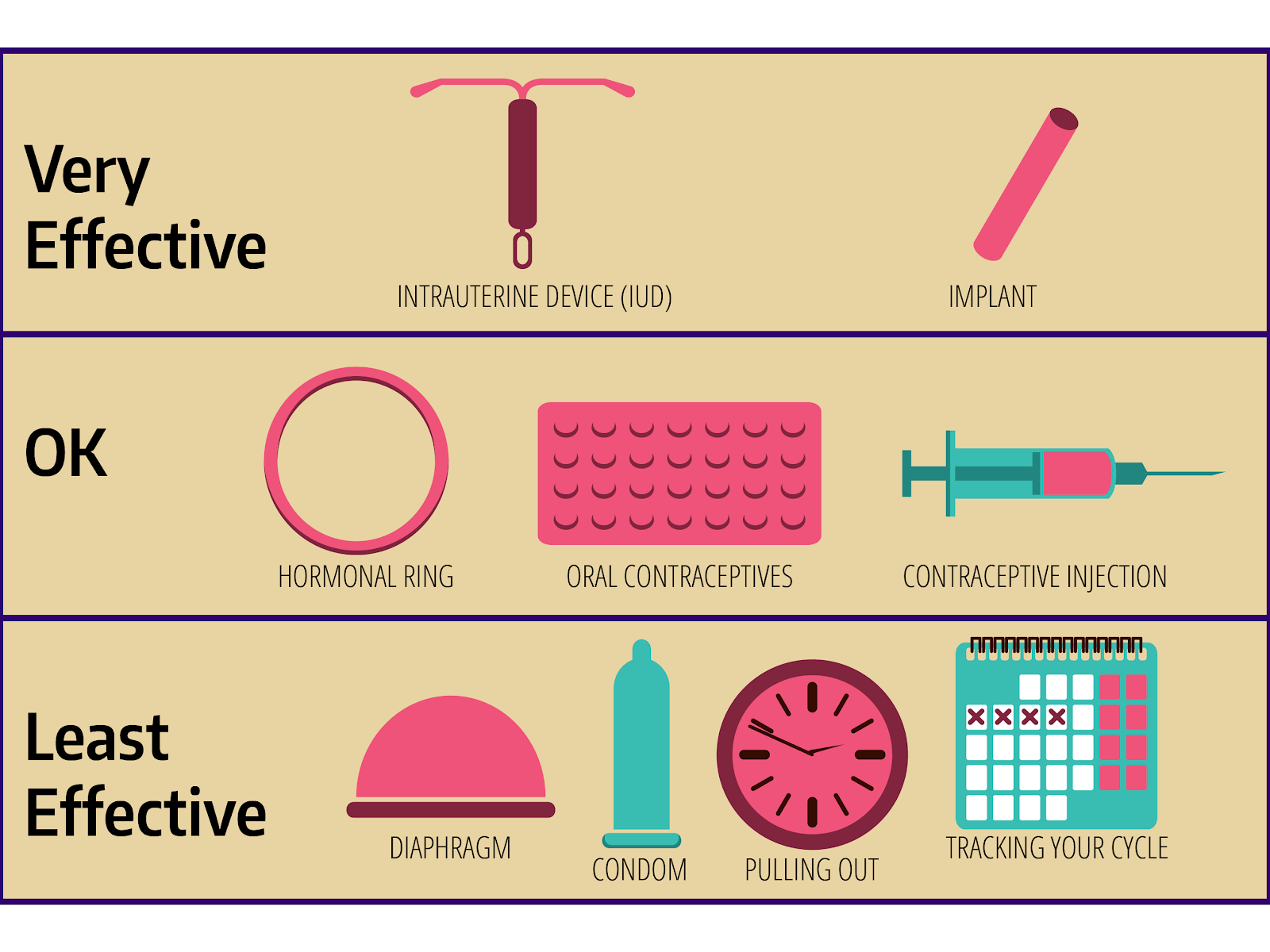
Birth Control Methods
Here are some of the most common birth control techniques:
What is hormonal birth control and how effective is it?
Hormonal birth control refers to a type of birth control that uses hormones to prevent pregnancy. It works by suppressing ovulation, thickening the cervical mucus, and altering the lining of the uterus to prevent implantation of a fertilized egg.
There are several types of hormonal birth control available, including:
- Combination hormonal birth control: This type of birth control combines estrogen and progestin (a synthetic version of the hormone progesterone) to prevent pregnancy.
- Progestin-only hormonal birth control: This type of birth control uses only progestin to prevent pregnancy.
- Minipills: These are small doses of estrogen and progestin that are taken daily to prevent pregnancy.
- Hormonal intrauterine devices (IUDs): These are small devices that are inserted into the uterus and release a steady stream of hormones to prevent pregnancy.
The effectiveness of hormonal birth control depends on several factors, including:
- Type of hormonal birth control used: Combination hormonal birth control is generally more effective than progestin-only hormonal birth control.
- Method of use: Taking the pills at the same time every day, not missing doses, and using back-up methods (such as condoms) can improve the effectiveness of hormonal birth control.
- User factors: Factors such as age, body weight, and smoking habits can affect the effectiveness of hormonal birth control.
According to the Centers for Disease Control and Prevention (CDC), the typical failure rate for combination hormonal birth control is around 0.1-0.3% per year. This means that out of 100 women who use combination hormonal birth control correctly, one or two may still become pregnant each year.
For progestin-only hormonal birth control, the typical failure rate is around 5-10% per year.
It’s important to note that hormonal birth control is not 100% effective and can fail due to various factors, including:
- Missing doses
- Taking pills at the wrong time
- Having a change in hormone levels (e.g., during pregnancy or while breastfeeding)
- Having certain medical conditions (e.g., liver disease or high blood pressure)
- Using other medications that interact with hormonal birth control
It’s important to discuss the effectiveness of hormonal birth control with your healthcare provider and to use it as part of a comprehensive reproductive health plan.
What are barrier birth control methods, and how effective are they?
Barrier birth control methods are a type of contraception that prevents sperm from reaching the egg by physically blocking the cervix. They are also known as mechanical barriers or physical barriers. Here are some examples of barrier birth control methods:
- Condoms: Made of latex or polyurethane, condoms are worn over the penis during sexual intercourse. They are effective in preventing pregnancy and sexually transmitted infections (STIs).
- Female condoms: Also known as internal condoms, these are made of thin, flexible material and are worn inside the vagina during sexual intercourse.
- Diaphragms: A flexible, dome-shaped device made of silicone or latex that is inserted into the vagina before sexual intercourse.
- Cervical caps: Small, soft cups made of silicone or latex that are inserted into the cervix before sexual intercourse.
- Vaginal barriers: These are small, flexible devices made of silicone or latex that are inserted into the vagina before sexual intercourse.
The effectiveness of barrier birth control methods depends on several factors, including:
- Proper use: If the barrier is not used correctly, it can be less effective.
- Type of barrier: Different types of barriers have different failure rates.
- User factors: Factors such as age, body weight, and smoking habits can affect the effectiveness of barrier birth control methods.
Here are some general effectiveness rates for barrier birth control methods:
- Condoms: 98-99% effective in preventing pregnancy, but 12-15% effective in preventing STIs.
- Female condoms: 95-98% effective in preventing pregnancy, but 95-100% effective in preventing STIs.
- Diaphragms: 92-96% effective in preventing pregnancy.
- Cervical caps: 80-90% effective in preventing pregnancy.
- Vaginal barriers: 80-90% effective in preventing pregnancy.
It’s important to note that barrier birth control methods are not foolproof and can fail if not used correctly or if there is a problem with the device itself. It’s also important to use a combination of methods, such as a condom and a spermicide, to increase the effectiveness of your birth control method.
What are some intrauterine devices and how effective are they?
Intrauterine devices (IUDs) are small, T-shaped devices that are inserted into the uterus to prevent pregnancy. There are several types of IUDs, including:
- Hormonal IUDs: These devices release a small amount of hormone, such as levonorgestrel or etonogestrel, into the uterus to prevent pregnancy. Examples of hormonal IUDs include:
- Mirena: Releases 20 micrograms of levonorgestrel per day and is effective for up to 5 years.
- Skyla: Releases 17.5 micrograms of levonorgestrel per day and is effective for up to 3 years.
- Liletta: Releases 10 micrograms of levonorgestrel per day and is effective for up to 3 years.
- Kyleena: Releases 19.5 micrograms of etonogestrel per day and is effective for up to 5 years.
- Non-hormonal IUDs: These devices do not release hormones and instead work by creating a physical barrier that prevents sperm from reaching the egg. Examples of non-hormonal IUDs include:
- Copper-T: A copper-based IUD that is effective for up to 10 years.
- ParaGard: A copper-based IUD that is effective for up to 10 years.
- Intrauterine balloon device (IUB): A small, inflatable balloon that is inserted into the uterus to prevent pregnancy.
The effectiveness of IUDs depends on several factors, including the type of IUD, the woman’s age, and the presence of any underlying medical conditions. Generally, hormonal IUDs are more effective than non-hormonal IUDs.
Here are some general effectiveness rates for IUDs:
- Hormonal IUDs: 99-99.9% effective in preventing pregnancy.
- Non-hormonal IUDs: 95-98% effective in preventing pregnancy.
It’s important to note that while IUDs are highly effective, they are not 100% effective and can fail if not used correctly or if there is a problem with the device itself. Additionally, IUDs can have some side effects, such as bleeding, cramping, and mood changes, although these are generally mild and temporary.
What are some natural methods of birth control and how effective are they?
There are several natural methods of birth control that have been used for centuries, including:
- Rhythm method: This method involves tracking the woman’s menstrual cycle to determine when she is most fertile and avoiding sexual intercourse during that time.
- Basal body temperature method: This method involves tracking the woman’s basal body temperature to determine when she is most fertile and avoiding sexual intercourse during that time.
- Cervical mucus method: This method involves tracking the changes in the woman’s cervical mucus to determine when she is most fertile and avoiding sexual intercourse during that time.
- Withdrawal method: This method involves withdrawing the penis from the vagina before ejaculation to prevent sperm from entering the vagina.
- Fertility awareness method: This method involves tracking the woman’s menstrual cycle, basal body temperature, and cervical mucus to determine when she is most fertile and avoiding sexual intercourse during that time.
- Natural family planning (NFP): This method involves tracking the woman’s menstrual cycle and other physical signs to determine when she is most fertile and avoiding sexual intercourse during that time.
The effectiveness of natural methods of birth control depends on several factors, including:
- Correct use: The method must be used correctly and consistently to be effective.
- User factors: Factors such as age, body weight, and smoking habits can affect the effectiveness of natural methods.
- Type of method: Different methods have different effectiveness rates.
Here are some general effectiveness rates for natural methods:
- Rhythm method: 80-90% effective
- Basal body temperature method: 80-90% effective
- Cervical mucus method: 75-85% effective
- Withdrawal method: 70-80% effective
- Fertility awareness method: 70-85% effective
- Natural family planning (NFP): 70-85% effective
It’s important to note that natural methods of birth control are not foolproof and can fail if not used correctly or if there is a problem with the woman’s reproductive system. Additionally, natural methods may not be suitable for everyone, particularly those who have a history of irregular menstrual cycles or other reproductive health issues.
What are permanent sterilization methods of birth control and how effective are they?
Permanent sterilization methods of birth control are surgical procedures that render a person unable to have children. These procedures are considered permanent because they are intended to be irreversible, meaning that they cannot be reversed or undone.
There are two main types of permanent sterilization methods:
- Vasectomy: This is a surgical procedure that is performed on men. It involves cutting and sealing the vas deferens, which are the tubes that carry sperm from the testicles to the penis. This prevents sperm from being released during ejaculation, making it impossible for the man to father a child.
- Tubal ligation: This is a surgical procedure that is performed on women. It involves cutting and sealing the fallopian tubes, which are the tubes that connect the ovaries to the uterus. This prevents sperm from reaching the egg and fertilization from occurring, making it impossible for the woman to become pregnant.
The effectiveness of permanent sterilization methods is extremely high, with failure rates typically less than 1% in both men and women.
Here are some statistics on the effectiveness of permanent sterilization methods:
- Vasectomy: The failure rate for vasectomy is typically less than 1% per year. According to the American Urological Association, the cumulative failure rate for vasectomy is 0.15% at 5 years, 0.25% at 10 years, and 0.35% at 15 years.
- Tubal ligation: The failure rate for tubal ligation is typically less than 1% per year. According to the American College of Obstetricians and Gynecologists, the failure rate for tubal ligation is 0.2% per year.
It’s important to note that while permanent sterilization methods are highly effective, they are not without risks and complications. Men who undergo vasectomy may experience pain, swelling, and bleeding during and after the procedure, as well as potential complications such as infection or injury to surrounding structures. Women who undergo tubal ligation may experience similar complications, as well as potential risks such as bleeding, infection, and damage to nearby organs.
It’s also important to note that permanent sterilization methods are not reversible, which means that they cannot be undone if you change your mind or want to have children in the future. Therefore, it’s important to carefully consider the decision to undergo permanent sterilization before making a decision.
What is emergency birth control and how effective is it?
Emergency birth control, also known as emergency contraception or morning-after pill, is a type of contraception that can be used to prevent pregnancy after unprotected sex or if a regular form of contraception fails. There are several types of emergency birth control available, including:
- Levonorgestrel (Plan B, Plan B One-Step): This is a pill that contains the hormone levonorgestrel, which prevents pregnancy by delaying ovulation and preventing fertilization.
- Ulipristal acetate (Ella): This is a pill that contains the hormone ulipristal acetate, which works by blocking the hormone progesterone and preventing ovulation.
- Non-hormonal IUDs: These are small, T-shaped devices that are inserted into the uterus and can be used as emergency contraception.
- Copper IUDs: These are small, T-shaped devices that are inserted into the uterus and contain copper, which can be used as emergency contraception.
The effectiveness of emergency birth control depends on several factors, including:
- Timing: The sooner you take emergency birth control, the more effective it is. The effectiveness of emergency birth control decreases with time.
- Type of emergency birth control: Different types of emergency birth control have different effectiveness rates.
- User factors: Factors such as age, body weight, and smoking habits can affect the effectiveness of emergency birth control.
Here are some general effectiveness rates for emergency birth control:
- Levonorgestrel (Plan B): 80-90% effective in preventing pregnancy when taken within 72 hours of unprotected sex.
- Ulipristal acetate (Ella): 95-99% effective in preventing pregnancy when taken within 120 hours of unprotected sex.
- Non-hormonal IUDs: 99-99.9% effective in preventing pregnancy when inserted within 5 days of unprotected sex.
- Copper IUDs: 99-99.9% effective in preventing pregnancy when inserted within 5 days of unprotected sex.
It’s important to note that emergency birth control is not a substitute for regular contraception and should not be used as a regular method of birth control. It’s also important to talk to your healthcare provider about the risks and benefits of emergency birth control and to discuss other options for preventing pregnancy.