BPH (Benign Prostatic Hyperplasia): Symptoms, Causes, Treatment
What are the symptoms of benign prostatic hyperplasia?
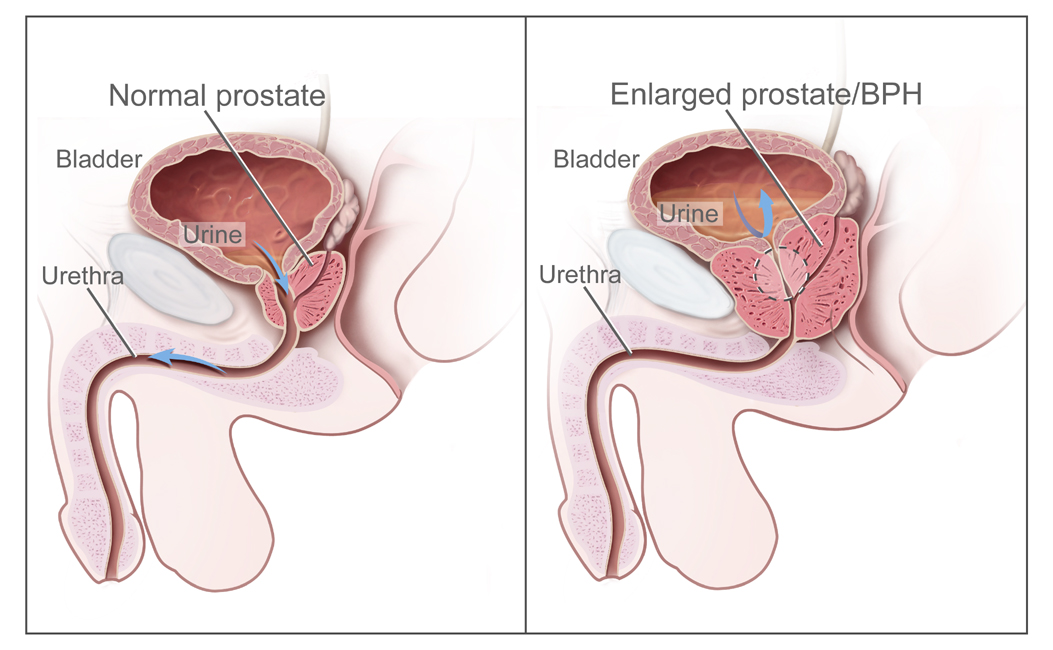
Benign prostatic hyperplasia (BPH), or an enlarged prostate gland, can cause a variety of urinary symptoms. Common symptoms include:
- Weak or interrupted urinary stream
The increased prostate size can compress the urethra, making it difficult to fully empty the bladder and causing a weak, inconsistent stream. - Frequent urination
As the bladder cannot empty completely, the urge to urinate comes more frequently, especially at night (nocturia). - Difficulty starting urination
The compressed urethra makes it harder to start the urine flow, leading to delays, hesitancy or straining to begin urinating. - Dribbling at the end of urination
Due to the obstruction, it’s hard to fully empty the bladder, causing dribbling after urination. - Feeling of incomplete bladder emptying
Even after urinating, there is a sensation that the bladder did not fully empty. - Urinary retention
In severe cases, the blockage can cause complete inability to urinate, requiring catheterization.
Other potential symptoms:
- Urgency to urinate
- Painful urination
- Blood in urine
- Urinary incontinence
- Urinary tract infections (UTIs)
The symptoms are often mild at first and progressively worsen over time as the prostate continues enlarging. Not all men with BPH experience symptoms. Severe, untreated BPH can potentially lead to complications like bladder stones, kidney damage or bladder failure.
What are the causes of benign prostatic hyperplasia?
Benign prostatic hyperplasia (BPH) or an enlarged prostate gland is mainly caused by hormonal changes that occur as men age. The primary causes and contributing factors include:
- Aging: BPH is rare in men younger than 40, but the incidence increases with age. The prostate gradually enlarges after age 25 and continues growing in most men during aging.
- Hormonal changes: The balance between testosterone and other hormones like dihydrotestosterone (DHT) and estrogen plays a key role. While testosterone levels fall with age, DHT levels may remain higher, promoting prostate cell growth.
- Cell accumulation: The prostate has two main cell types. As men age, the accumulation of these cells leads to prostate enlargement.
- Inflammation: Chronic inflammation within the prostate can stimulate cell multiplication and prostate enlargement over time.
- Ethnicity: BPH is more common in African-American men compared to Caucasian men.
- Family history: A genetic predisposition or inherited factors may influence prostate growth.
- Obesity and metabolic syndrome: These conditions can increase BPH risk, possibly due to hormonal effects.
While prostate enlargement is very common in aging men, only some develop symptoms or complications from BPH that require treatment. The degree of obstruction caused by the enlarged prostate determines the severity of symptoms.
Hormones play a permissive role in prostate growth, while other factors likely initiate or accelerate the process. Effective treatments target reducing prostate volume or relieving obstruction.
What is the treatment for benign prostatic hyperplasia?
There are several treatment options available for benign prostatic hyperplasia (BPH), depending on the severity of symptoms and the size of the prostate gland. The treatments aim to relieve urinary symptoms and reduce potential complications. Common treatments include:
Medications:
- Alpha-blockers (e.g. tamsulosin, doxazosin) – Relax prostate/bladder muscles to improve urine flow
- 5-alpha reductase inhibitors (e.g. finasteride, dutasteride) – Shrink enlarged prostate by blocking testosterone conversion
Minimally Invasive Therapies:
- Transurethral Needle Ablation (TUNA) – Uses radiofrequency energy to heat and destroy prostate tissue
- Transurethral Microwave Therapy (TUMT) – Microwave energy to ablate prostate tissue
- Prostatic Urethral Lift (UroLift) – Implants pull back prostate lobes to open urethra
Surgical Treatments:
- Transurethral Resection of the Prostate (TURP) – The most common surgery, removes blocking prostate tissue
- Laser surgery (HoLEP, GreenLight) – Laser energy vaporizes obstructive prostate tissue
- Open prostatectomy – Full or partial surgical removal of the prostate, for very large glands
- Transurethral incision of the prostate (TUIP) – Makes small cuts in the prostate to open urethra
Other Options:
- Watchful waiting/monitoring – For mild symptoms, deferring treatment with regular monitoring
- Lifestyle changes – Avoiding alcohol/caffeine, double voiding, scheduled voiding
- Urinary catheters – For acute urinary retention when conservative options fail
The choice depends on factors like prostate size, severity of symptoms, age, overall health and preferences. Minimally invasive therapies are often tried before invasive surgery. Combining medications with other treatments is also common.