Brazilian Pemphigus Foliaceus: Symptoms, Causes & Treatment
What are the symptoms of Brazilian pemphigus foliaceus?
Brazilian pemphigus foliaceus is a rare autoimmune skin disease that primarily affects the skin. The main symptoms of Brazilian pemphigus foliaceus include:
- Skin blisters and erosions: The most characteristic symptom is the development of fragile, fluid-filled blisters and erosions on the skin. These typically start on the face, scalp, and upper trunk before spreading to other areas of the body.
- Crusting and scaling: As the blisters rupture, they leave behind areas of raw, exposed skin that can crust over and develop thick, yellow scales.
- Skin peeling: The blisters and erosions can lead to widespread peeling or shedding of the outer layer of skin (superficial epidermis).
- Itching and burning sensation: Patients often experience intense itching, burning, or stinging sensations in the affected areas.
- Skin infections: The raw, exposed areas of skin are susceptible to secondary bacterial or fungal infections, which can worsen the symptoms and lead to additional complications.
- Hair loss: In some cases, blisters and erosions can develop on the scalp, leading to patchy hair loss or alopecia.
- Nail changes: Nail abnormalities, such as ridging, discoloration, or nail shedding, may occur in some patients.
- Mucous membrane involvement: Unlike other forms of pemphigus, Brazilian pemphigus foliaceus typically does not affect the mucous membranes of the mouth, nose, or genitals.
The severity of symptoms can vary widely among individuals, ranging from mild and localized to widespread and severe. Prompt diagnosis and treatment are important to manage the symptoms, prevent complications, and improve the patient’s quality of life.
What are the causes of Brazilian pemphigus foliaceus?
The primary cause of Brazilian pemphigus foliaceus is an autoimmune reaction in which the body’s immune system mistakenly attacks and destroys the desmoglein-1 (Dsg1) protein, which is responsible for holding the outer layer of skin cells (keratinocytes) together. Several factors are thought to contribute to the development of this autoimmune response:
- Genetic predisposition: Certain genetic factors, particularly variations in the human leukocyte antigen (HLA) system, which regulates the immune response, are believed to increase an individual’s susceptibility to developing Brazilian pemphigus foliaceus.
- Environmental triggers: Various environmental factors, such as exposure to certain medications, viruses (e.g., herpes simplex virus), ultraviolet radiation, or physical trauma, may trigger the autoimmune response in genetically predisposed individuals.
- Molecular mimicry: Some researchers suggest that the immune system may mistake the Dsg1 protein for a foreign antigen, such as a viral or bacterial protein, leading to the production of autoantibodies against Dsg1.
- Epitope spreading: Once the autoimmune response is initiated against a specific epitope (part) of the Dsg1 protein, it may spread to other epitopes, amplifying the autoimmune attack.
- Geographic factors: Brazilian pemphigus foliaceus is more prevalent in certain regions, such as Brazil, Colombia, and parts of Central America, suggesting that environmental or genetic factors specific to these areas may play a role.
- Hormonal influences: Changes in hormonal levels, such as during pregnancy or menopause, have been associated with an increased risk or exacerbation of Brazilian pemphigus foliaceus in some cases.
It’s important to note that the exact mechanisms behind the development of this autoimmune condition are not fully understood, and multiple factors likely contribute to its initiation and progression.
What is the treatment for Brazilian pemphigus foliaceus?
The treatment for Brazilian pemphigus foliaceus aims to control the autoimmune reaction, prevent the formation of new blisters and erosions, and promote healing of the affected skin areas. The main treatment approaches include:
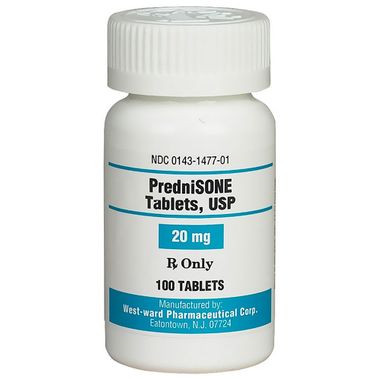
- Corticosteroids:
- Oral corticosteroids, such as prednisone or prednisolone, are the primary treatment for Brazilian pemphigus foliaceus.
- These drugs help suppress the abnormal immune response and reduce inflammation.
- Topical corticosteroids may also be used for localized lesions.
- Immunosuppressants:
- In severe cases or when corticosteroids alone are insufficient, other immunosuppressive medications may be added, such as azathioprine, mycophenolate mofetil, or cyclophosphamide.
- These drugs help further suppress the autoimmune response and allow for lower doses of corticosteroids.
- Rituximab:
- Rituximab is a monoclonal antibody that selectively targets and depletes B cells, which produce the autoantibodies responsible for the disease.
- It has shown promising results in treating refractory cases of Brazilian pemphigus foliaceus.
- Intravenous immunoglobulin (IVIG):
- IVIG can help modulate the immune response and may be used as an adjunct therapy in severe or refractory cases.
- Supportive care:
- Proper wound care, including topical antiseptics and dressings, is important to prevent infections and promote healing.
- Antihistamines and pain medication may be prescribed to manage itching and discomfort.
- Nutritional support and hydration are essential for patients with extensive skin involvement.
- Sun protection:
- Avoiding sun exposure and using broad-spectrum sunscreens can help prevent flare-ups triggered by ultraviolet radiation.
The treatment plan is tailored to each individual based on the severity of the disease, response to therapy, and potential side effects. Close monitoring and regular follow-up are necessary to adjust the treatment as needed and manage any complications.
In some cases, remission can be achieved with appropriate treatment, but relapses are common, and long-term maintenance therapy may be required to prevent further flare-ups.