Breast Cancer & Genes
The chances of carrying a breast cancer gene, specifically mutations in the BRCA1 and BRCA2 genes, depend on several factors including your personal and family medical history. Here are some factors that may increase your likelihood of carrying a breast cancer gene mutation:
- Family history: A strong family history of breast cancer, especially if it occurs at an early age (before age 50) or if multiple family members are affected, may indicate an increased risk of carrying a genetic mutation.
- Personal history: If you have been diagnosed with breast cancer at a young age, have had multiple primary breast cancers, or have a history of other cancers such as ovarian cancer, your risk of carrying a genetic mutation may be higher.
- Ethnicity: Certain ethnic populations, such as individuals of Ashkenazi Jewish descent, have a higher prevalence of BRCA mutations compared to the general population.
- Genetic counseling and testing: If you are concerned about your risk of carrying a breast cancer gene mutation, genetic counseling and testing can help assess your risk. A genetic counselor can review your personal and family medical history, discuss the benefits and limitations of genetic testing, and help you make informed decisions about testing.
It’s important to note that most cases of breast cancer are not caused by inherited genetic mutations, but rather by a combination of genetic, lifestyle, and environmental factors. Only about 5-10% of breast cancer cases are attributed to inherited genetic mutations, such as BRCA1 and BRCA2.
If you are considering genetic testing for breast cancer gene mutations, it is recommended to speak with a healthcare provider or genetic counselor who can help you understand the implications of testing, interpret the results, and provide guidance on cancer screening, prevention, and treatment options based on your individual risk profile. Early detection and personalized risk management strategies can help reduce the risk of developing breast cancer or improve outcomes if cancer is detected.
How do I examine myself for breast cancer?
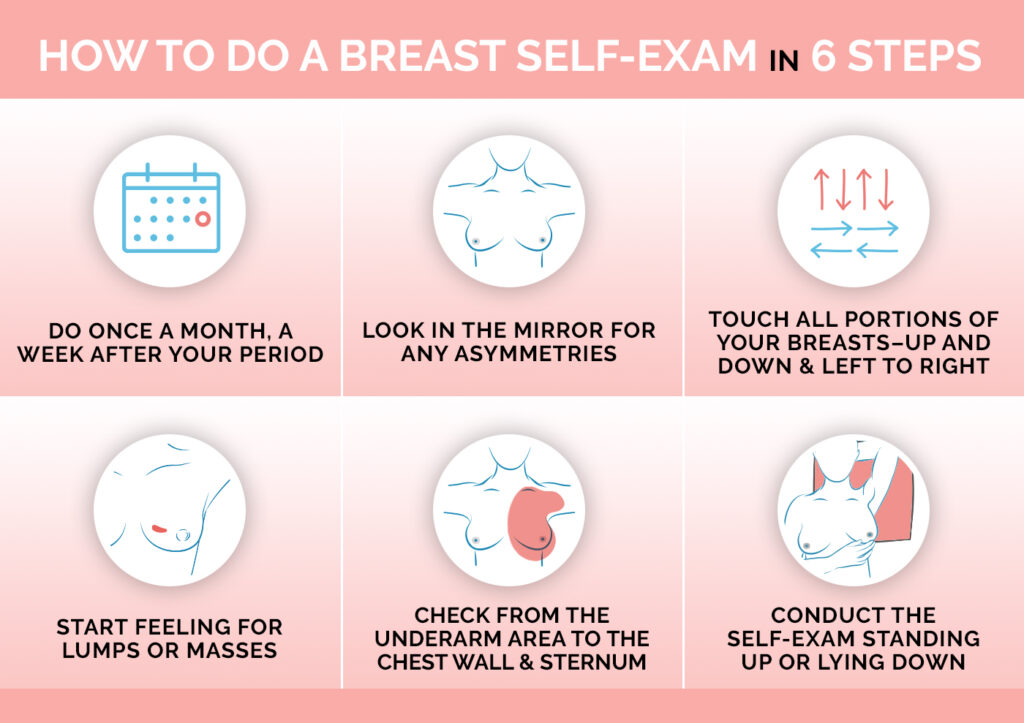
Self-examination for breast cancer, often referred to as a breast self-exam (BSE), can be a useful way to become familiar with the normal look and feel of your breasts so that you can detect any changes early. Here’s a basic guide to performing a breast self-exam:
- Choose a regular time: Perform the exam at the same time each month, such as a few days after your period ends, when your breasts are least likely to be swollen or tender.
- Stand or sit in front of a mirror: Look for any changes in the size, shape, or contour of your breasts, as well as any dimpling, puckering, or redness of the skin. Check for changes in the nipples, such as inversion, discharge, or scaling.
- Raise your arms: Look for the same changes as in step 2 with your arms raised overhead.
- Lie down: Use your right hand to feel your left breast and vice versa. Use the pads of your fingers, keeping them flat and together. Use a circular motion about the size of a quarter and cover the entire breast from top to bottom, side to side, from your collarbone to the top of your abdomen, and from your armpit to your cleavage. Apply light, medium, and firm pressure to feel the different depths of breast tissue.
- Feel for lumps: Pay special attention to any lumps, hard knots, or thickening in your breasts or underarm area.
- Repeat on the other breast: Repeat the same process for the other breast.
- Check for discharge: Gently squeeze each nipple to check for discharge. Normal discharge is usually clear or milky in color.
It’s important to note that most breast lumps are not cancerous. However, if you notice any changes in your breasts, such as a new lump, swelling, pain, or nipple discharge, it’s important to see a healthcare provider for further evaluation. Regular screening mammograms are also recommended for women over a certain age or at higher risk for breast cancer.
See also: