Breast Lumps: Causes & Treatments
What are the common causes of breast lumps?
There are several common causes of breast lumps in women:
- Fibrocystic changes
This is a benign (non-cancerous) condition where lumpy, dense tissue or cysts develop in the breasts, often related to hormonal changes. It is very common and affects over half of women. - Fibroadenoma
These are solid, benign lumps made up of breast gland and connective tissue. They are movable and most common in younger women. - Cysts
Fluid-filled sacs or cysts can develop in the breast tissue, forming smooth, mobile lumps. They often enlarge and become tender before menstrual periods. - Breast cancer
While much less common than benign causes, a lump can potentially be a sign of breast cancer, especially if it feels hard, immobile and asymmetric. - Mastitis
An infection in the breast tissue during breastfeeding can cause a painful, irregular lump to form. - Traumatic fat necrosis
This develops after a breast injury, forming a firm lump from damaged fatty breast tissue. - Intraductal papilloma
A small, benign growth that develops in the milk ducts near the nipple can feel like a firm lump.
Other less common causes include abscess, hematoma, lipoma, or phyllodes tumor.
Most breast lumps end up being non-cancerous, especially in younger women. However, any new or changing lump should be evaluated promptly by a doctor through clinical exam, imaging tests like ultrasound or mammogram, and potentially biopsy to determine the cause definitively.
What should I do if I find a breast lump?
If you discover a new lump or mass in your breast, it’s important to get it evaluated by a medical professional promptly. Here are the recommended steps to take:
- Don’t panic. Many breast lumps end up being benign (non-cancerous), especially in younger women. But you should still get it checked out.
- Note the details. Make note of the lump’s size, location in the breast, texture (hard, soft, movable), and if there’s any nipple discharge or skin changes.
- Schedule an exam. Call your doctor’s office and schedule a clinical breast exam as soon as possible. Describe the lump and your concerns.
- Get diagnostic imaging. After examining the lump, your doctor will likely order breast imaging tests like a mammogram, ultrasound, or both to get a better look.
- Consider additional tests. If the imaging looks suspicious, you may need additional tests like a biopsy to remove cells/tissue from the lump for laboratory analysis.
- Don’t try to remove it yourself. Don’t poke, squeeze or massage the lump, as this can lead to bleeding, bruising or infection.
- Discuss your risk factors. Let your doctor know about any personal or family history of breast cancer that may increase your risk.
- Follow up as recommended. Depending on the findings, you may need routine monitoring, follow-up imaging, or prompt treatment if breast cancer is diagnosed.
The key is to have any new, unusual breast lumps evaluated without delay by a doctor, who can order the proper imaging and testing to determine the cause. Early detection is important for effective treatment if it is breast cancer.
How often should I get a mammogram?
The recommendations for how often to get a mammogram can vary slightly based on different medical organizations, but here are some general guidelines:
For Women at Average Risk:
- Age 40-44: Annual mammograms are an option to consider
- Age 45-54: Annual mammograms are recommended
- Age 55 and older: Mammograms every 1-2 years
These recommendations assume you are at average risk for breast cancer with no personal history or strong family history of the disease.
For Women at Higher Risk:
- Start annual mammograms at an earlier age, typically around 30-35 years old
- Get supplemental breast MRI scans along with mammograms
- Discuss optimal screening schedule with your doctor based on your specific risk factors
Higher risk includes having a BRCA gene mutation, a first-degree relative with breast cancer, personal history of breast cancer or certain breast conditions.
Additional Considerations:
- Continue mammograms as long as you are in good health
- Clinical breast exams every 1-3 years from age 25-39, then annually from age 40
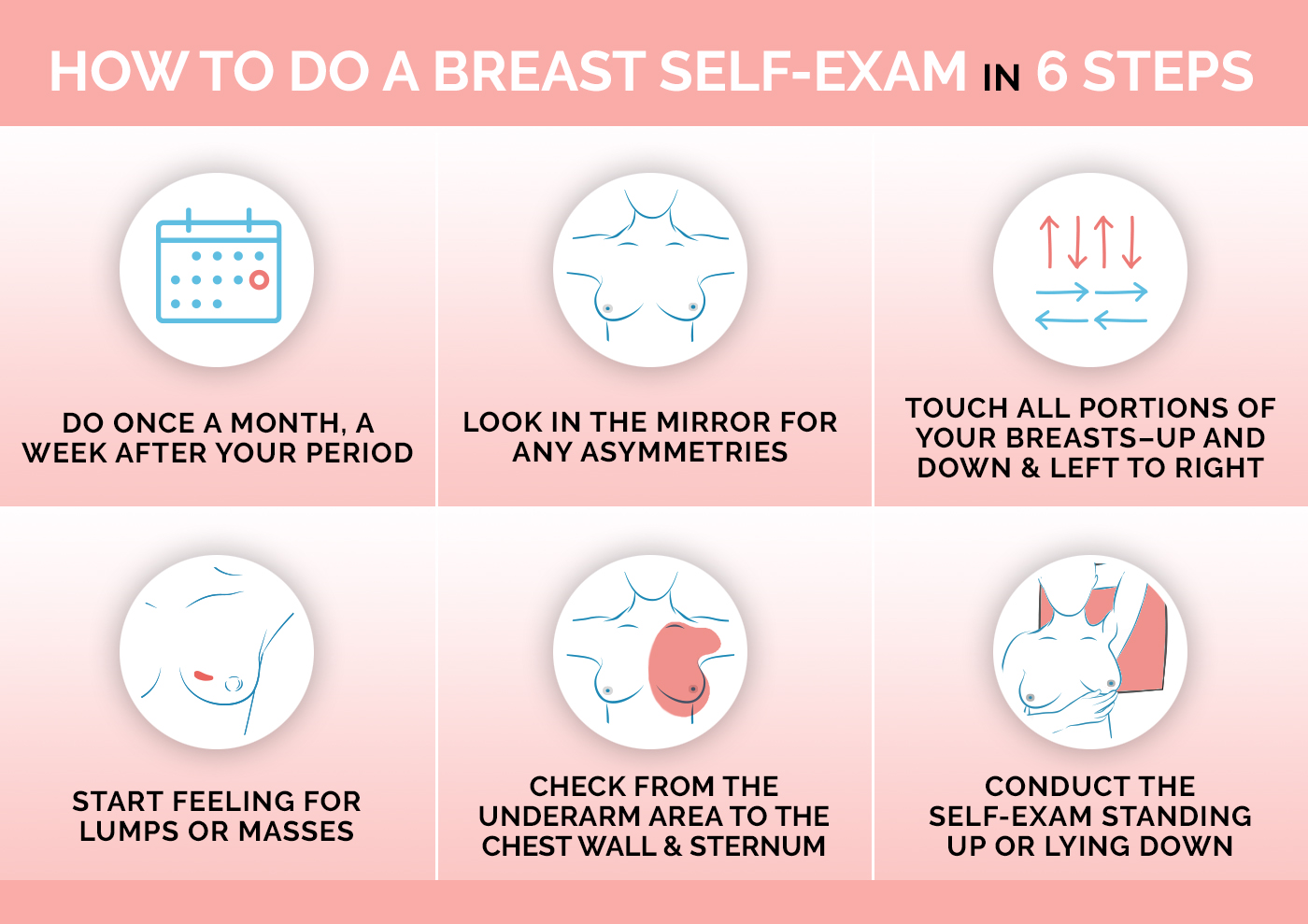
- Breast self-exams are an option to become familiar with how your breasts normally look/feel
The goal is to maximize early detection while minimizing risks from over-screening. Your doctor may recommend a more or less frequent schedule based on your individual breast cancer risk assessment.
It’s important to talk to your doctor about the benefits and limitations of mammograms and establish a screening plan that provides you with the best breast health monitoring based on your age and risk profile.