Congestive Heart Failure: Symptoms, Causes, Treatment
What are the symptoms of congestive heart failure?
Congestive heart failure (CHF), also known as heart failure, is a chronic condition in which the heart is unable to pump enough blood to meet the body’s needs. This can lead to a buildup of fluid in the body and a variety of symptoms. The symptoms of congestive heart failure can vary depending on the severity of the condition and which side of the heart is affected (left side, right side, or both). Common symptoms of congestive heart failure include:
- Shortness of breath: One of the hallmark symptoms of congestive heart failure is shortness of breath, especially during physical activity or when lying flat. This is often due to fluid buildup in the lungs (pulmonary congestion).
- Fatigue: Feeling tired or fatigued, even after rest, is common in congestive heart failure. This can be due to reduced blood flow and oxygen delivery to the body’s tissues.
- Swelling: Fluid buildup (edema) can cause swelling in the legs, ankles, feet, or abdomen. This swelling may be more noticeable at the end of the day or after periods of sitting or standing.
- Weight gain: Sudden or unexplained weight gain can be a sign of fluid retention due to congestive heart failure.
- Increased heart rate: The heart may beat faster than normal (tachycardia) to try to compensate for its reduced pumping ability.
- Persistent cough: A cough that produces white or pink blood-tinged mucus may occur due to fluid buildup in the lungs.
- Wheezing or chest tightness: These symptoms may occur due to fluid buildup in the lungs or underlying lung conditions exacerbated by heart failure.
- Decreased exercise tolerance: Difficulty performing regular activities or reduced exercise capacity may be a symptom of congestive heart failure.
- Loss of appetite: Some people with congestive heart failure may experience a loss of appetite or nausea, which can contribute to weight loss.
- Confusion or impaired thinking: In severe cases, congestive heart failure can lead to mental confusion or impaired thinking due to reduced blood flow to the brain.
It’s important to note that the symptoms of congestive heart failure can be similar to those of other conditions, so a thorough evaluation by a healthcare provider is necessary for an accurate diagnosis and appropriate treatment. If you experience any of these symptoms, especially if they are new or worsening, it’s important to seek medical attention promptly.
What are the causes of congestive heart failure?
Congestive heart failure (CHF) can be caused by a variety of underlying conditions that affect the heart’s ability to pump blood effectively. Some common causes and contributing factors to congestive heart failure include:
- Coronary artery disease (CAD): CAD is a condition in which the arteries that supply blood to the heart become narrowed or blocked due to a buildup of plaque. This can lead to a heart attack, which can damage the heart muscle and impair its ability to pump blood effectively.
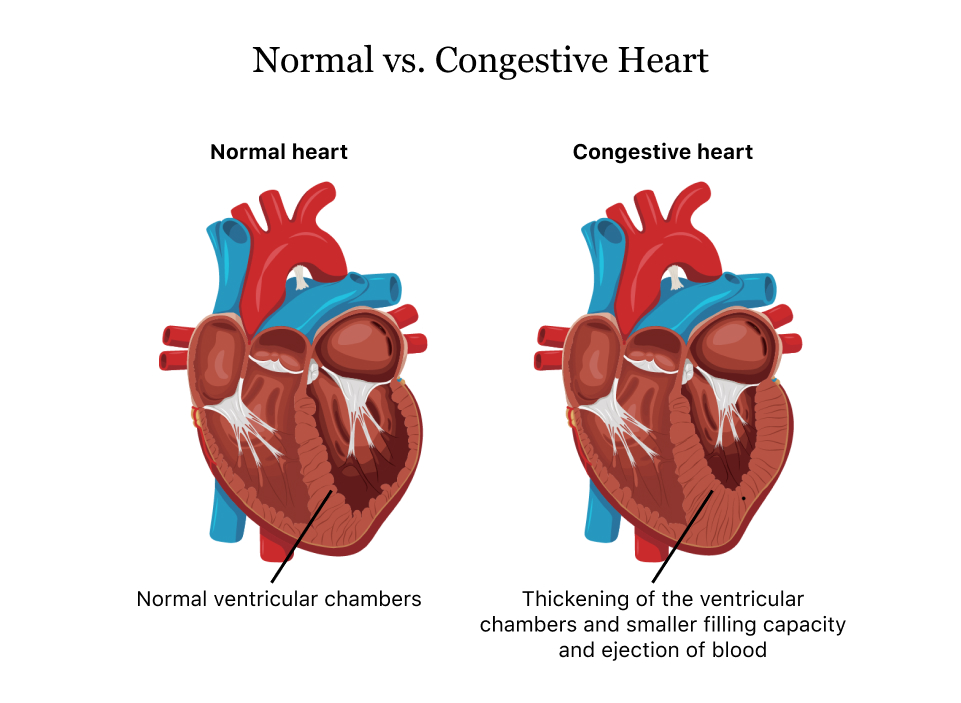
- High blood pressure (hypertension): Chronic high blood pressure can cause the heart to work harder to pump blood, leading to enlargement of the heart muscle (left ventricular hypertrophy) and eventual weakening of the heart muscle.
- Cardiomyopathy: Cardiomyopathy refers to diseases of the heart muscle that can weaken the heart and impair its ability to pump blood effectively. There are several types of cardiomyopathy, including dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy.
- Valvular heart disease: Diseases of the heart valves, such as aortic stenosis or mitral regurgitation, can impair the heart’s ability to pump blood effectively, leading to congestive heart failure.
- Myocarditis: Myocarditis is inflammation of the heart muscle, often due to a viral infection. It can weaken the heart muscle and impair its ability to pump blood effectively.
- Arrhythmias: Abnormal heart rhythms (arrhythmias) can disrupt the heart’s pumping function and lead to congestive heart failure.
- Congenital heart defects: Some people are born with structural abnormalities of the heart that can lead to congestive heart failure later in life.
- Other factors: Other factors that can contribute to or worsen congestive heart failure include diabetes, obesity, thyroid disorders (hypothyroidism, hyperthyroidism), kidney disease, and certain medications.
It’s important to note that congestive heart failure can result from a combination of these factors, and the specific cause may vary among individuals. Treatment for congestive heart failure typically focuses on addressing the underlying cause, managing symptoms, and improving quality of life.
What is the treatment for congestive heart failure?
The treatment for congestive heart failure (CHF) aims to improve the heart’s function, reduce symptoms, prevent complications, and improve quality of life. Treatment options may include:
- Lifestyle changes: Adopting a heart-healthy lifestyle can help manage CHF. This includes maintaining a healthy weight, eating a balanced diet low in sodium, exercising regularly, quitting smoking, and limiting alcohol intake.
- Medications: Several medications are used to treat CHF, including:
- Angiotensin-converting enzyme (ACE) inhibitors: These help relax blood vessels, lower blood pressure, and improve blood flow.
- Beta-blockers: These help reduce heart rate, blood pressure, and the heart’s workload.
- Diuretics: These help reduce fluid buildup and swelling.
- Aldosterone antagonists: These help reduce fluid buildup and improve heart function.
- Angiotensin II receptor blockers (ARBs): These are an alternative to ACE inhibitors for some people.
- Devices: In some cases, devices may be recommended to help improve heart function. These include:
- Implantable cardioverter-defibrillator (ICD): This device can help regulate heart rhythm and prevent sudden cardiac arrest.
- Cardiac resynchronization therapy (CRT): This involves the implantation of a device that helps coordinate the contractions of the heart’s chambers.
- Ventricular assist devices (VADs): These devices help pump blood from the heart to the rest of the body and are sometimes used as a bridge to heart transplantation.
- Surgery: In some cases, surgery may be recommended to treat underlying heart conditions that contribute to CHF. This may include coronary artery bypass surgery, heart valve repair or replacement, or heart transplant.
- Monitoring and follow-up care: Regular monitoring by a healthcare provider is important to assess heart function, adjust medications, and address any changes in symptoms. This may include regular check-ups, blood tests, and imaging tests.
- End-of-life care: For individuals with advanced CHF, palliative care or hospice care may be appropriate to help manage symptoms and improve quality of life.
The specific treatment plan for CHF will depend on the underlying cause, the severity of the condition, and the individual’s overall health. It’s important for individuals with CHF to work closely with a healthcare provider to develop a comprehensive treatment plan that addresses their specific needs and goals.