Crohn’s Disease: Symptoms, Causes, Treatment
What are the symptoms of Crohn’s disease?
Crohn’s disease is a chronic inflammatory condition that primarily affects the digestive tract, although it can also cause symptoms outside the digestive tract. The symptoms of Crohn’s disease can vary widely among individuals, but common symptoms may include:
- Abdominal pain and cramping: This is one of the most common symptoms of Crohn’s disease and is often located in the lower right abdomen.
- Diarrhea: Chronic diarrhea is another hallmark symptom of Crohn’s disease, which may be bloody in some cases.
- Weight loss: Reduced appetite, diarrhea, and malabsorption of nutrients can lead to weight loss in individuals with Crohn’s disease.
- Fatigue: Chronic inflammation and nutrient deficiencies can lead to fatigue and weakness.
- Fever: Some individuals with Crohn’s disease may experience low-grade fevers.
- Mouth sores: Some people with Crohn’s disease may develop mouth sores, similar to canker sores.
- Reduced appetite: Loss of appetite is common in Crohn’s disease, especially during flare-ups.
- Perianal symptoms: Crohn’s disease can cause symptoms around the anus, including fistulas (abnormal tunnels between the intestine and skin), abscesses, and skin tags.
- Joint pain: Some individuals with Crohn’s disease may experience joint pain or swelling, which is often similar to arthritis.
- Skin problems: Crohn’s disease can cause skin problems such as red, tender bumps (erythema nodosum) or painful, red skin lesions (pyoderma gangrenosum).
- Eye inflammation: Crohn’s disease can cause inflammation in the eyes, leading to symptoms such as redness, pain, or blurred vision.
It’s important to note that the symptoms of Crohn’s disease can vary in severity and may come and go over time. Additionally, not all individuals with Crohn’s disease will experience all of these symptoms. If you suspect you have Crohn’s disease, it’s important to see a healthcare provider for proper diagnosis and management.
What are the causes of Crohn’s disease?
The exact cause of Crohn’s disease is not yet fully understood, but it is believed to involve a combination of genetic, environmental, and immune system factors. Some potential causes and risk factors include:
- Genetics: Crohn’s disease tends to run in families, suggesting that there may be a genetic component. Several genetic mutations have been identified that may increase the risk of developing Crohn’s disease.
- Immune system dysfunction: In people with Crohn’s disease, the immune system may mistakenly attack harmless bacteria in the digestive tract, leading to inflammation and damage to the intestinal lining.
- Environmental factors: Certain environmental factors, such as smoking, diet, and exposure to certain infections, may increase the risk of developing Crohn’s disease. However, the role of these factors is not yet fully understood.
- Abnormal gut microbiome: Changes in the composition of the gut microbiome (the community of bacteria and other microorganisms in the digestive tract) may play a role in the development of Crohn’s disease.
- Smoking: Smoking is a significant risk factor for developing Crohn’s disease, as it can worsen the course of the disease and increase the risk of complications.
- Autoimmune response: Some researchers believe that Crohn’s disease may be caused by an abnormal immune response, where the immune system attacks healthy cells in the digestive tract.
- Previous infections: Previous infections with certain bacteria or viruses may trigger an abnormal immune response that leads to Crohn’s disease in susceptible individuals.
It’s important to note that while these factors may increase the risk of developing Crohn’s disease, they do not guarantee that a person will develop the condition. The exact cause of Crohn’s disease is likely to be complex and multifactorial, and more research is needed to fully understand its underlying causes.
What is the treatment for Crohn’s disease?
The treatment for Crohn’s disease aims to reduce inflammation, control symptoms, and improve quality of life. The specific treatment approach may vary depending on the severity of the disease, the location of inflammation, and the individual’s response to treatment. Some common treatments for Crohn’s disease include:
- Medications:
- Anti-inflammatory drugs: such as corticosteroids (e.g., prednisone), mesalamine, and immunomodulators (e.g., azathioprine, 6-mercaptopurine) to reduce inflammation.
- Biologic therapies: such as anti-tumor necrosis factor (TNF) drugs (e.g., infliximab, adalimumab) and other biologic agents (e.g., vedolizumab, ustekinumab) to target specific parts of the immune system.
- Antibiotics: to treat bacterial overgrowth or infections in the digestive tract.
- Anti-diarrheal medications: to help control diarrhea.
- Nutritional therapy:
- Exclusive enteral nutrition (EEN): a liquid diet that provides complete nutrition and may help reduce inflammation in the digestive tract.
- Elemental diet: a liquid diet that provides easily digestible nutrients.
- Supplemental nutrition: to address nutritional deficiencies that may occur due to malabsorption.
- Surgery: In severe cases or when complications arise, surgery may be necessary to remove damaged portions of the digestive tract or repair fistulas, strictures, or other complications.
- Lifestyle modifications:
- Dietary changes: Some individuals find that certain foods can trigger or worsen symptoms. Keeping a food diary may help identify and avoid these triggers.
- Stress management: Stress can worsen symptoms, so stress-reducing techniques such as yoga, meditation, or counseling may be beneficial.
- Monitoring and follow-up: Regular monitoring by a healthcare provider is important to assess disease activity, adjust treatment as needed, and screen for complications such as malnutrition, osteoporosis, and colorectal cancer.
It’s important for individuals with Crohn’s disease to work closely with a healthcare provider to develop a personalized treatment plan that addresses their specific symptoms and needs. Treatment may need to be adjusted over time based on the individual’s response to therapy and the course of the disease.
Crohn’s Disease Summary
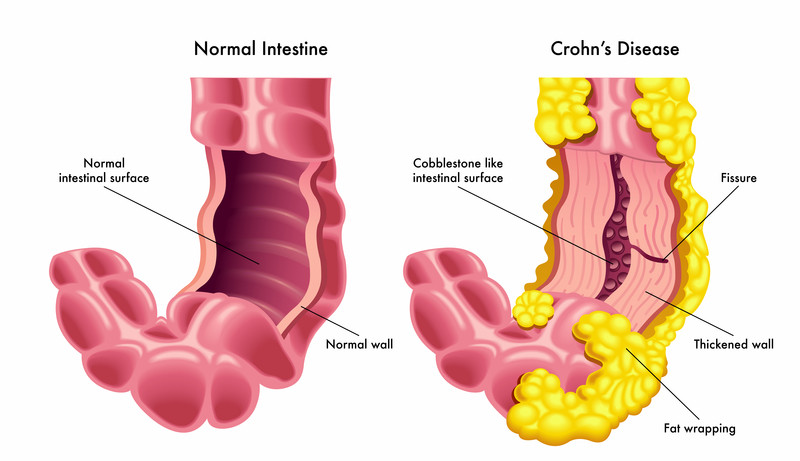
Crohn’s disease is a chronic inflammatory condition that primarily affects the gastrointestinal tract, most commonly the small intestine and the colon. It is part of a group of conditions known as inflammatory bowel diseases (IBD), which also includes ulcerative colitis. Crohn’s disease causes inflammation in the lining of the digestive tract, leading to symptoms such as abdominal pain, diarrhea, fatigue, weight loss, and malnutrition.
The exact cause of Crohn’s disease is not well understood, but it is believed to involve a combination of genetic, environmental, and immune system factors. People with a family history of Crohn’s disease are at a higher risk of developing the condition. Additionally, factors such as smoking, diet, and certain medications may play a role in triggering or exacerbating the disease.
Symptoms of Crohn’s disease can vary depending on the location and severity of the inflammation, and they may come and go over time. Common symptoms include abdominal pain and cramping, diarrhea (sometimes bloody), fatigue, weight loss, reduced appetite, fever, and inflammation of the skin, eyes, or joints.
Diagnosing Crohn’s disease typically involves a combination of medical history, physical examination, blood tests, imaging studies (such as CT scans or MRIs), and endoscopic procedures (such as colonoscopy or flexible sigmoidoscopy) to examine the lining of the gastrointestinal tract.
Treatment for Crohn’s disease focuses on controlling inflammation, reducing symptoms, preventing complications, and improving quality of life. Treatment options may include medications (such as anti-inflammatory drugs, immunosuppressants, or biologic therapies), dietary modifications, lifestyle changes, and, in some cases, surgery to remove damaged portions of the intestine. Crohn’s disease is a chronic condition that requires ongoing management and monitoring by healthcare providers to optimize long-term outcomes.