Cutaneous T-Cell Lymphomas: Symptoms, Causes, Treatment
What are the symptoms of cutaneous T-cell lymphomas?
Cutaneous T-cell lymphomas (CTCL) are a group of rare cancers that affect the skin and occur when certain white blood cells called T-cells become cancerous and grow uncontrollably. The symptoms of CTCL can vary depending on the type and stage of the disease, but common symptoms may include:
- Skin rash or lesions: The most common symptom of CTCL is a persistent, itchy rash that may resemble eczema or psoriasis. The rash may appear as red, scaly patches or plaques on the skin.
- Thickened skin: In some cases, the skin affected by CTCL may become thickened, hardened, or leathery in texture.
- Skin tumors: As the disease progresses, tumors or nodules may develop on the skin. These tumors are usually painless but may ulcerate or bleed.
- Lymph node enlargement: In advanced stages of CTCL, the cancerous T-cells may spread to the lymph nodes, causing them to enlarge.
- Symptoms of advanced disease: In later stages of CTCL, when the cancer has spread beyond the skin, symptoms may include fatigue, weight loss, and generalized itching.
It’s important to note that the symptoms of CTCL can be similar to those of other skin conditions, so a proper diagnosis by a dermatologist or oncologist is essential. If you experience any persistent skin changes or symptoms that concern you, it’s important to seek medical attention for an accurate diagnosis and appropriate treatment.
What are the causes of cutaneous T-cell lymphomas?
The exact cause of cutaneous T-cell lymphomas (CTCL) is not well understood. Like other types of cancer, CTCL is thought to develop as a result of genetic mutations that cause normal cells to become cancerous. However, the specific genetic mutations or factors that lead to the development of CTCL are not fully known.
Some factors that may play a role in the development of CTCL include:
- Immune system dysfunction: CTCL is more common in individuals with weakened immune systems, such as those with HIV/AIDS or those who have undergone organ transplantation and are taking immunosuppressive medications. This suggests that an abnormal immune response may contribute to the development of CTCL.
- Genetic predisposition: There may be a genetic component to the development of CTCL, as the disease sometimes runs in families. However, the specific genes involved have not been identified.
- Environmental factors: Some studies suggest that certain environmental factors, such as exposure to certain chemicals or pollutants, may increase the risk of developing CTCL. However, more research is needed to understand the role of environmental factors in the development of the disease.
- Viral infections: Some researchers have investigated the role of viral infections, such as the human T-cell lymphotropic virus (HTLV-1), in the development of CTCL. However, the relationship between viral infections and CTCL is not well understood.
Overall, the development of CTCL is likely to be multifactorial, involving a combination of genetic, environmental, and immune-related factors. Further research is needed to better understand the causes of CTCL and develop more effective treatments.
What is the treatment for cutaneous T-cell lymphomas?
The treatment for cutaneous T-cell lymphomas (CTCL) depends on several factors, including the type and stage of the disease, the individual’s overall health, and their preferences. Treatment options for CTCL may include:
- Topical treatments: For early-stage CTCL, when the disease is limited to the skin, topical treatments such as corticosteroids, retinoids, or topical chemotherapy may be used to help control skin symptoms.
- Phototherapy: Phototherapy, which involves exposing the skin to ultraviolet (UV) light, can be an effective treatment for CTCL. Types of phototherapy used for CTCL include PUVA (psoralen plus UVA) and narrow-band UVB therapy.
- Systemic treatments: For more advanced or aggressive CTCL, systemic treatments that affect the entire body may be used. These may include:
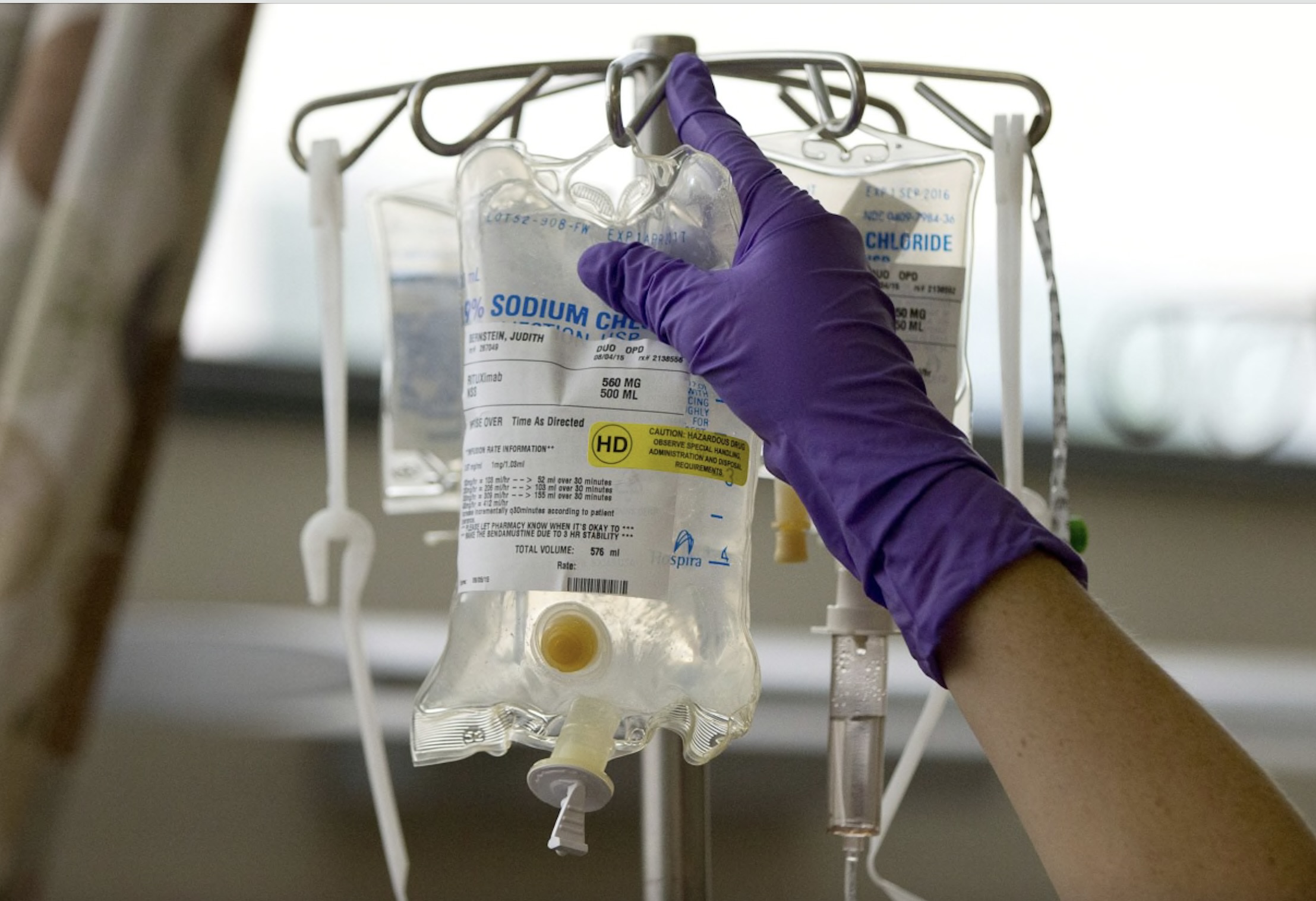
- Chemotherapy: Chemotherapy drugs may be used to kill cancer cells and slow the progression of the disease.
- Biological therapy: Biological therapies, such as interferon or monoclonal antibodies, may be used to target specific proteins on cancer cells or to boost the immune system’s response to the cancer.
- Targeted therapy: Targeted therapies, such as vorinostat or romidepsin, may be used to target specific genetic mutations or pathways involved in the growth of cancer cells.
- Immunotherapy: Immunotherapy drugs, such as checkpoint inhibitors, may be used to help the immune system recognize and attack cancer cells.
- Radiation therapy: Radiation therapy may be used to target and destroy cancer cells in a specific area of the skin or lymph nodes.
- Stem cell transplant: In some cases, a stem cell transplant may be recommended for individuals with advanced CTCL. This involves replacing diseased bone marrow with healthy stem cells to help the body produce healthy blood cells.
- Clinical trials: Participation in clinical trials may be an option for some individuals with CTCL. Clinical trials test new treatments or treatment combinations to determine their safety and effectiveness.
The choice of treatment for CTCL depends on several factors, and a healthcare provider specializing in lymphoma or dermatology can help determine the most appropriate treatment plan. Treatment for CTCL is often ongoing, and regular follow-up visits are important to monitor the response to treatment and manage any side effects.