Diabetic Macular Edema: Symptoms, Causes & Treatment
What are the symptoms of diabetic macular edema?
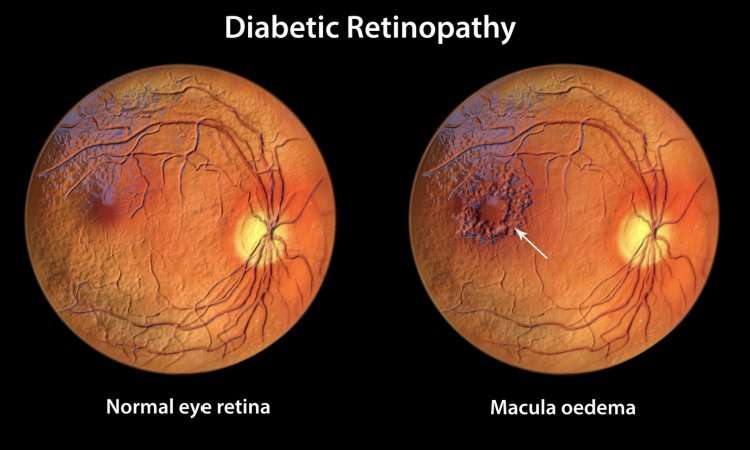
Diabetic macular edema (DME) is a complication of diabetic retinopathy, a condition that affects the blood vessels in the retina. DME occurs when fluid leaks from blood vessels into the macula, the central part of the retina responsible for sharp, central vision. The symptoms of DME may include:
- Blurred or Distorted Vision: Blurred vision is a common symptom of DME. Some people may also experience distorted or wavy vision.
- Difficulty Reading or Seeing Fine Details: DME can make it difficult to read or see fine details clearly.
- Floaters: Floaters are spots or dark strings that appear to float in the field of vision. They may be a sign of bleeding in the eye (vitreous hemorrhage), which can occur in advanced cases of DME.
- Decreased Color Sensitivity: Some people with DME may notice a decrease in their ability to see colors vividly.
- Vision Loss: In severe cases, DME can lead to partial or total vision loss if left untreated.
It’s important for people with diabetes to have regular eye exams to detect diabetic retinopathy and DME early, when treatment is most effective. If you experience any of these symptoms, especially if they are new or worsening, it’s important to see an eye care professional for an evaluation. Early detection and treatment of DME can help prevent vision loss and preserve vision.
What is the cause of diabetic macular edema?
Diabetic macular edema (DME) is caused by damage to the blood vessels in the retina, which occurs as a result of long-term high blood sugar levels in people with diabetes. The exact cause of DME is not fully understood, but it is believed to be related to the following factors:
- Leaky Blood Vessels: High blood sugar levels can damage the blood vessels in the retina, causing them to become leaky. When fluid leaks from these blood vessels into the macula, the central part of the retina responsible for sharp, central vision, it can lead to swelling and thickening of the macula, resulting in DME.
- Inflammation: Inflammation in the retina can contribute to the development of DME. High blood sugar levels and other factors associated with diabetes can lead to inflammation in the eye, which can contribute to the leakage of fluid from blood vessels.
- Vascular Endothelial Growth Factor (VEGF): VEGF is a protein that plays a key role in the growth of new blood vessels. In people with diabetes, high levels of VEGF can contribute to the growth of abnormal blood vessels in the retina and the leakage of fluid into the macula, leading to DME.
- Ischemia: Ischemia refers to reduced blood flow to the retina, which can occur as a result of damage to the blood vessels. Ischemia can lead to the release of factors that promote the growth of abnormal blood vessels and the leakage of fluid into the macula.
- Other Factors: Other factors, such as high blood pressure, high cholesterol levels, and smoking, can also contribute to the development of DME in people with diabetes.
Managing blood sugar levels, blood pressure, and cholesterol levels, as well as quitting smoking, can help reduce the risk of developing DME. Regular eye exams are also important for detecting DME early, when treatment is most effective.
What is the treatment for diabetic macular edema?
The treatment for diabetic macular edema (DME) aims to reduce swelling in the macula, improve vision, and prevent further vision loss. The treatment options for DME may include:
- Anti-VEGF Injections: Anti-VEGF medications, such as bevacizumab (Avastin), ranibizumab (Lucentis), and aflibercept (Eylea), can be injected into the eye to help reduce swelling and improve vision. These injections are typically given on a regular schedule, often monthly or as needed based on the response to treatment.
- Corticosteroid Injections: Corticosteroids, such as triamcinolone acetonide or dexamethasone, can be injected into the eye to help reduce inflammation and swelling in the macula. These injections may be used alone or in combination with anti-VEGF medications.
- Laser Photocoagulation: Laser treatment (photocoagulation) can be used to seal leaking blood vessels in the retina or to reduce swelling in the macula. Laser treatment is typically used in cases where anti-VEGF injections are not effective or as a secondary treatment.
- Vitrectomy: In severe cases of DME, a vitrectomy may be performed. This surgical procedure involves removing the vitreous gel from the eye to allow for better visualization and treatment of the retina.
- Steroid Implants: Tiny steroid implants can be placed in the eye to release medication over time and reduce swelling in the macula. These implants may be used in cases where frequent injections are not feasible.
- Monitoring and Follow-Up: Regular monitoring of vision and eye health is important for managing DME. Follow-up appointments with an eye care professional are necessary to monitor the response to treatment and make any necessary adjustments.
It’s important for people with DME to work closely with their healthcare team, including an eye care professional, to develop a treatment plan that meets their individual needs. Early detection and treatment of DME can help prevent vision loss and preserve vision.
See also: