Diabetic Nephropathy: Symptoms, Causes, Treatment
What are the symptoms of diabetic nephropathy?
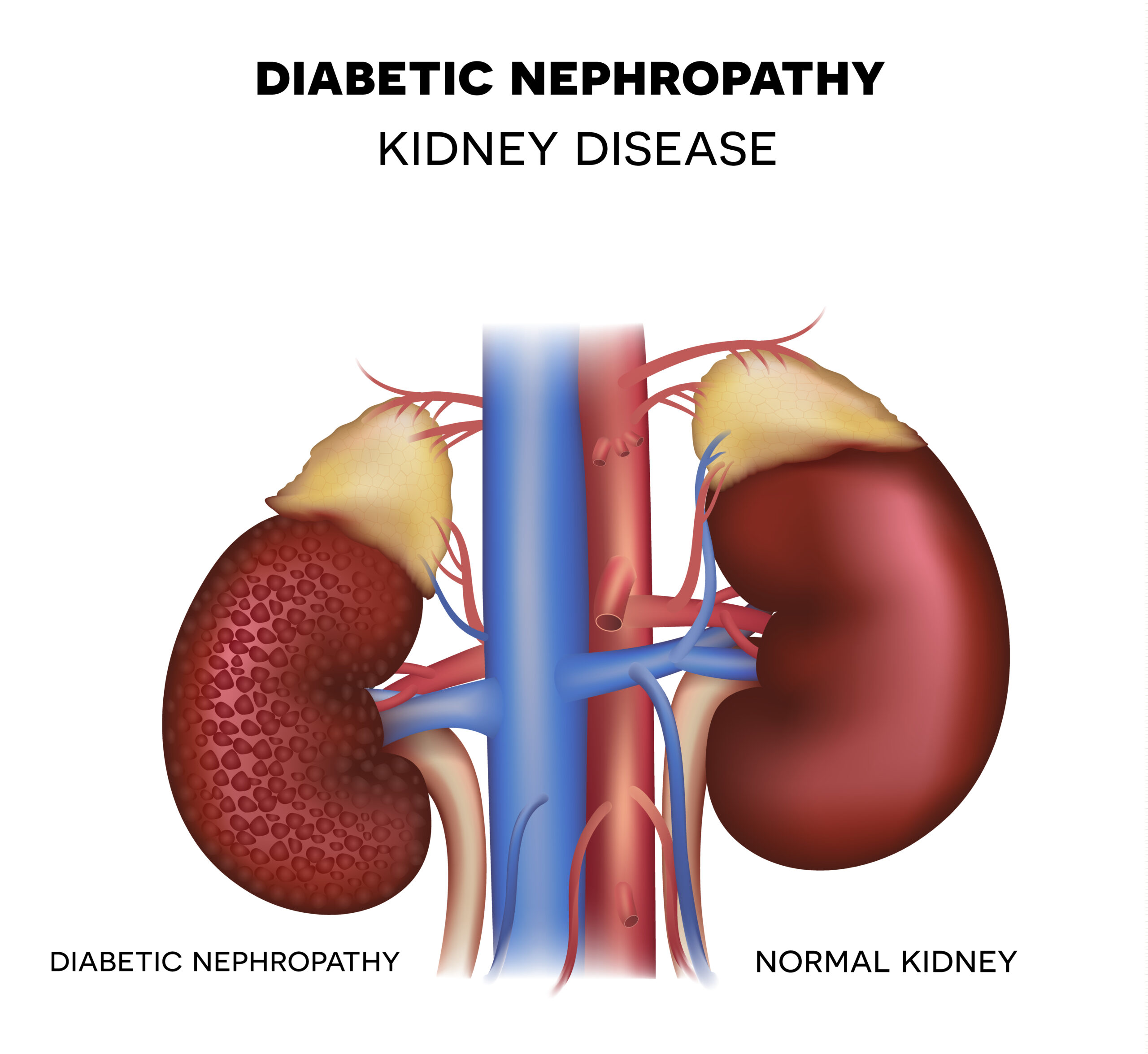
Diabetic nephropathy, also known as diabetic kidney disease, is a complication of diabetes that affects the kidneys. In its early stages, diabetic nephropathy may not cause any noticeable symptoms. However, as the condition progresses, symptoms may develop. The symptoms of diabetic nephropathy may include:
- Swelling (Edema): Swelling, usually in the legs, ankles, feet, or hands, due to fluid retention caused by the kidneys’ inability to filter waste products properly.
- Foamy Urine: Urine that appears foamy or bubbly, which may be a sign of proteinuria (excess protein in the urine).
- Increased Urination: An increase in the frequency of urination, especially at night (nocturia), or an increase in the amount of urine produced.
- Fatigue: Unexplained fatigue or weakness, which may be due to anemia (a low red blood cell count) caused by kidney damage.
- Loss of Appetite: A decrease in appetite or unexplained weight loss.
- Nausea and Vomiting: Nausea, vomiting, or a general feeling of illness.
- Itching (Pruritus): Itching, often severe, due to the build-up of waste products in the blood.
- Muscle Cramps: Muscle cramps, especially in the legs, which may occur due to electrolyte imbalances caused by kidney dysfunction.
- High Blood Pressure (Hypertension): High blood pressure is common in people with diabetic nephropathy and may be a sign of kidney damage.
- Changes in Skin Color: Changes in the color of the skin, especially in the legs or feet, which may appear pale or darker than usual.
It’s important to note that these symptoms can also be caused by other conditions, and having one or more of these symptoms does not necessarily mean you have diabetic nephropathy. However, if you have diabetes and experience any of these symptoms, it’s important to see a healthcare provider for evaluation and appropriate testing. Early detection and management of diabetic nephropathy can help slow the progression of kidney damage and reduce the risk of complications.
What are the causes of diabetic nephropathy?
Diabetic nephropathy, also known as diabetic kidney disease, is a complication of diabetes that occurs when high blood sugar levels damage the kidneys’ filtering units, called nephrons. Several factors contribute to the development of diabetic nephropathy:
- Chronic High Blood Sugar Levels: Prolonged periods of high blood sugar levels (hyperglycemia) can damage the small blood vessels in the kidneys and impair their ability to filter waste products from the blood.
- Hypertension (High Blood Pressure): High blood pressure is a common complication of diabetes and can further damage the kidneys’ blood vessels, worsening diabetic nephropathy.
- Genetics: Some people may be genetically predisposed to developing diabetic nephropathy. Family history of kidney disease or diabetes may increase the risk.
- Smoking: Smoking can accelerate the progression of diabetic nephropathy and increase the risk of kidney damage.
- Obesity: Excess body weight, particularly abdominal obesity, is a risk factor for diabetic nephropathy.
- Poorly Controlled Blood Sugar Levels: Inadequate management of diabetes, including failure to take medications as prescribed, follow a healthy diet, or engage in regular physical activity, can increase the risk of diabetic nephropathy.
- Duration of Diabetes: The longer a person has had diabetes, the higher their risk of developing diabetic nephropathy. However, not everyone with diabetes will develop kidney disease.
- Other Factors: Other factors that may increase the risk of diabetic nephropathy include age, ethnicity (African Americans, Hispanics, and Native Americans are at higher risk), and certain medical conditions such as cardiovascular disease.
It’s important for individuals with diabetes to monitor their blood sugar levels regularly, follow a healthy lifestyle, and manage other risk factors such as high blood pressure and cholesterol to reduce the risk of developing diabetic nephropathy. Early detection and treatment of diabetic nephropathy are crucial to slowing its progression and preventing complications.
What is the treatment for diabetic nephropathy?
The treatment for diabetic nephropathy focuses on controlling blood sugar levels, managing blood pressure, and reducing the risk of complications. Treatment may include:
- Blood Sugar Control: Tight control of blood sugar levels through diet, exercise, and medication is essential to slow the progression of diabetic nephropathy. This may involve monitoring blood sugar levels regularly and adjusting insulin or other medications as needed.
- Blood Pressure Management: Keeping blood pressure under control is crucial in managing diabetic nephropathy. This may involve lifestyle changes (such as reducing salt intake, losing weight, and exercising regularly) and medications to lower blood pressure.
- Medications: Medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) are often used to treat diabetic nephropathy. These medications help protect the kidneys and lower blood pressure.
- Cholesterol Management: Controlling cholesterol levels through diet, exercise, and medications if necessary can help reduce the risk of complications from diabetic nephropathy.
- Healthy Diet: A healthy diet low in salt, saturated fats, and processed sugars can help manage blood sugar levels and reduce the risk of complications.
- Regular Exercise: Regular physical activity can help control blood sugar levels, lower blood pressure, and improve overall health.
- Smoking Cessation: Quitting smoking can help slow the progression of diabetic nephropathy and reduce the risk of complications.
- Regular Monitoring: Regular monitoring of kidney function, blood sugar levels, blood pressure, and cholesterol levels is important for managing diabetic nephropathy and preventing complications.
In some cases, more advanced treatments may be necessary, such as dialysis or kidney transplantation, if kidney function becomes severely impaired. It’s important for individuals with diabetic nephropathy to work closely with their healthcare team to develop a personalized treatment plan and monitor their condition regularly. Early detection and management of diabetic nephropathy can help slow its progression and reduce the risk of complications.