Ear Infection: Symptoms, Causes, Treatment
What are the symptoms of an ear infection?
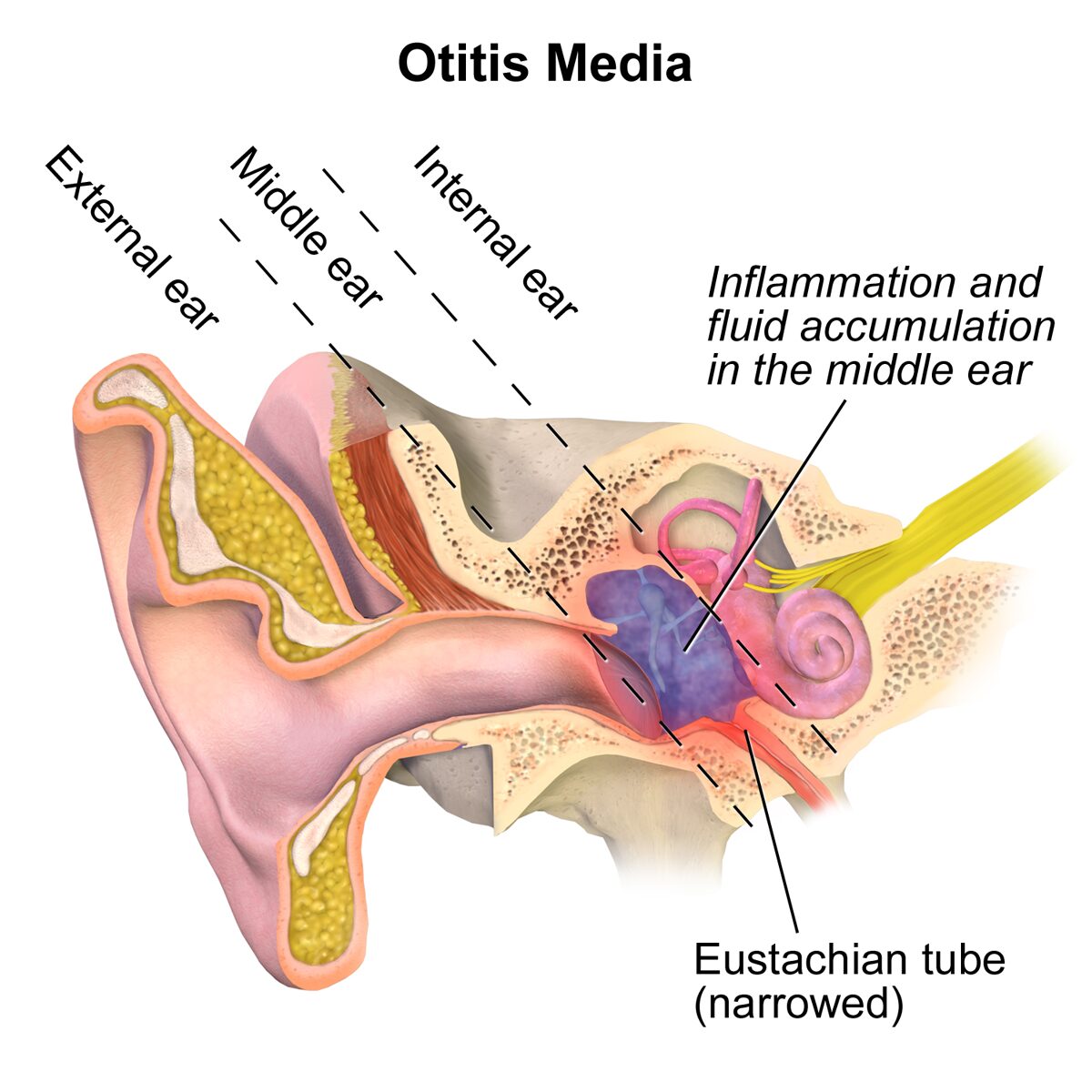
Ear infections, also known as otitis media, can occur in the middle ear (the space behind the eardrum) or the outer ear. The symptoms of an ear infection can vary depending on the type of infection and its severity, but common symptoms may include:
- Ear Pain: Ear pain is a common symptom of an ear infection, especially in children. The pain may be sharp, dull, or throbbing and may be worse when lying down.
- Ear Drainage: Some people with ear infections may experience drainage from the ear. The drainage may be clear, yellow, or bloody and may indicate a ruptured eardrum.
- Hearing Loss: Temporary hearing loss or muffled hearing may occur due to fluid buildup in the middle ear.
- Fever: A fever is often present, especially in cases of middle ear infections.
- Feeling of Fullness: Some individuals may experience a feeling of fullness or pressure in the ear.
- Irritability (in infants and young children): Ear infections can cause irritability, fussiness, and difficulty sleeping in infants and young children.
- Balance Problems: In some cases, an ear infection can affect balance and coordination, leading to dizziness or vertigo.
- Headache: Some people with ear infections may experience headaches, especially if the infection is severe or if there is associated sinus congestion.
It’s important to note that not everyone with an ear infection will experience all of these symptoms, and the severity of symptoms can vary. If you or your child experience symptoms of an ear infection, it’s important to see a healthcare provider for evaluation and appropriate management.
What are the causes of an ear infection?
Ear infections are typically caused by bacteria or viruses that infect the middle ear, the space behind the eardrum. The most common causes of ear infections include:
- Bacterial Infection: The most common bacteria that cause ear infections are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. These bacteria can enter the middle ear through the Eustachian tube, which connects the middle ear to the back of the throat.
- Viral Infection: Viruses such as respiratory syncytial virus (RSV), influenza virus, and adenovirus can also cause ear infections, especially in young children.
- Eustachian Tube Dysfunction: The Eustachian tube helps equalize pressure in the middle ear. Dysfunction of the Eustachian tube, often due to allergies, colds, or sinus infections, can lead to fluid buildup in the middle ear, creating a favorable environment for bacteria or viruses to grow.
- Anatomical Factors: Certain anatomical factors, such as a cleft palate or a narrow Eustachian tube, can increase the risk of ear infections.
- Environmental Factors: Exposure to tobacco smoke, high levels of air pollution, or living in crowded conditions can increase the risk of ear infections.
- Age: Ear infections are more common in children, particularly those between the ages of 6 months and 2 years, due to the size and shape of their Eustachian tubes.
- Seasonal Factors: Ear infections are more common in the fall and winter months, when respiratory infections are more prevalent.
It’s important to note that not all ear infections are caused by bacteria. Viral ear infections are also common, especially in cases where the infection accompanies a viral respiratory infection. Treatment for ear infections may vary depending on the cause and severity of the infection.
What is the treatment for an ear infection?
The treatment for an ear infection depends on the type of infection and its severity. In many cases, the infection will resolve on its own without treatment. However, if symptoms are severe or if the infection is caused by bacteria, treatment may be necessary. Treatment options for ear infections may include:
- Pain Relief: Over-the-counter pain relievers such as acetaminophen or ibuprofen may help relieve ear pain and fever associated with an ear infection.
- Antibiotics: If the ear infection is caused by bacteria, a healthcare provider may prescribe antibiotics to help clear the infection. It’s important to take the full course of antibiotics as prescribed, even if symptoms improve before the medication is finished.
- Ear Drops: Ear drops containing antibiotics or steroids may be prescribed to help reduce inflammation and clear the infection.
- Warm Compress: Applying a warm compress to the affected ear may help relieve pain and discomfort.
- Eardrum Incision: In some cases, a healthcare provider may make a small incision in the eardrum to drain fluid from the middle ear and relieve pressure.
- Tympanostomy Tubes: In cases of recurrent ear infections or persistent fluid buildup, a healthcare provider may recommend placing small tubes in the eardrums to help drain fluid and prevent future infections.
- Observation: In some cases, especially with mild ear infections, a healthcare provider may recommend a “wait-and-see” approach, where symptoms are monitored closely without immediate treatment.
It’s important to follow your healthcare provider’s recommendations for treatment and to seek medical attention if symptoms worsen or do not improve with treatment. Untreated ear infections can lead to complications such as hearing loss, so it’s important to address them promptly.