Eaton-Lambert Syndrome: Symptoms, Causes, Treatment
What are the symptoms of Eaton-Lambert syndrome?
Eaton-Lambert syndrome, also known as Lambert-Eaton myasthenic syndrome (LEMS), is a rare autoimmune disorder that affects the neuromuscular junction, the point where nerves and muscles meet. The primary symptom of LEMS is muscle weakness, which typically affects the muscles closest to the trunk of the body, such as the hips, thighs, shoulders, and upper arms. Other symptoms may include:
- Muscle Weakness: The hallmark symptom of LEMS is muscle weakness, which is often more pronounced after periods of rest or inactivity and improves with repeated use of the affected muscles.
- Difficulty Walking: Weakness in the legs and hips can make it difficult to walk or climb stairs, and some individuals may experience a waddling gait.
- Fatigue: Fatigue is a common symptom of LEMS and can be both physical and mental in nature.
- Autonomic Dysfunction: Some individuals with LEMS may experience symptoms related to autonomic dysfunction, such as dry mouth, constipation, and changes in blood pressure and heart rate.
- Difficulty Speaking or Swallowing: Weakness in the muscles involved in speech and swallowing can lead to difficulty speaking clearly or swallowing food and liquids.
- Double Vision (Diplopia): Weakness in the muscles that control eye movements can cause double vision.
- Reduced Reflexes: A characteristic feature of LEMS is reduced or absent reflexes, which can be detected during a physical exam.
- Pain: Some individuals with LEMS may experience muscle pain, cramps, or aching, especially after physical activity.
It’s important to note that the symptoms of LEMS can vary widely among individuals, and not everyone will experience all of these symptoms. Additionally, the symptoms of LEMS can overlap with other neuromuscular disorders, so a thorough evaluation by a healthcare provider is necessary for an accurate diagnosis.
What are the causes of Eaton-Lambert syndrome?
Eaton-Lambert syndrome, or Lambert-Eaton myasthenic syndrome (LEMS), is an autoimmune disorder in which the immune system mistakenly attacks the neuromuscular junction, the point where nerves and muscles meet. This attack leads to dysfunction in the communication between nerves and muscles, resulting in muscle weakness and other symptoms. The exact cause of LEMS is not fully understood, but it is believed to be associated with the following factors:
- Autoimmune Response: LEMS is thought to be an autoimmune disorder, meaning that the immune system mistakenly targets and attacks healthy tissues in the body. In LEMS, the immune system targets the neuromuscular junction, disrupting the normal communication between nerves and muscles.
- Voltage-Gated Calcium Channels: In most cases of LEMS, the immune system produces antibodies that target and attack voltage-gated calcium channels (VGCCs) in the neuromuscular junction. VGCCs play a crucial role in allowing nerve cells to release chemicals that signal muscles to contract. By targeting VGCCs, the immune system interferes with this signaling process, leading to muscle weakness.
- Paraneoplastic Syndrome: In some cases, LEMS may be associated with an underlying cancer, particularly small cell lung cancer. In these cases, the body’s immune response to the cancer cells may also contribute to the development of LEMS.
- Genetic Factors: While LEMS is not thought to be directly inherited, certain genetic factors may play a role in predisposing individuals to develop the condition.
It’s important to note that the exact cause of LEMS can vary among individuals, and in some cases, the underlying cause may not be identified. Treatment for LEMS typically focuses on managing symptoms and may include medications to improve muscle strength and function, as well as treatments to target the underlying autoimmune response.
What is the treatment for Eaton-Lambert syndrome?
The treatment for Eaton-Lambert syndrome (Lambert-Eaton myasthenic syndrome or LEMS) focuses on managing symptoms and improving muscle strength and function. Treatment options may include:
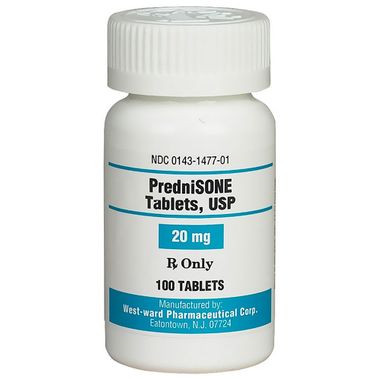
- Immunosuppressive Therapy: Medications that suppress the immune system, such as corticosteroids (e.g., prednisone) or immunosuppressants (e.g., azathioprine), may be used to reduce the immune system’s attack on the neuromuscular junction.
- Symptomatic Treatment: Medications that improve muscle strength and function, such as 3,4-diaminopyridine (3,4-DAP) or pyridostigmine, may be prescribed to help improve muscle function and reduce weakness.
- Plasmapheresis: Plasmapheresis, also known as plasma exchange, may be used to remove antibodies from the bloodstream that are attacking the neuromuscular junction. This procedure can help improve muscle strength and function, but the effects are usually temporary and may need to be repeated.
- Intravenous Immunoglobulin (IVIG): IVIG is a treatment that involves infusing antibodies from donated blood into the bloodstream. IVIG can help modulate the immune response and reduce the attack on the neuromuscular junction, leading to improved muscle function.
- Physical Therapy: Physical therapy may be recommended to help improve muscle strength, mobility, and coordination. A physical therapist can provide exercises and techniques to help manage symptoms and improve quality of life.
- Treatment of Underlying Cancer: In cases where LEMS is associated with an underlying cancer, such as small cell lung cancer, treatment of the cancer may help improve symptoms of LEMS.
- Monitoring and Supportive Care: Regular monitoring by a healthcare provider is important to assess symptoms, monitor disease progression, and adjust treatment as needed. Supportive care, such as assistive devices or mobility aids, may also be beneficial in managing symptoms and improving quality of life.
It’s important for individuals with LEMS to work closely with their healthcare providers to develop a treatment plan that addresses their specific needs and symptoms. Treatment may need to be adjusted over time based on the individual’s response to therapy and disease progression.