Familial Congestive Cardiomyopathy: Symptoms, Causes, Treatment
What are the symptoms of familial congestive cardiomyopathy?
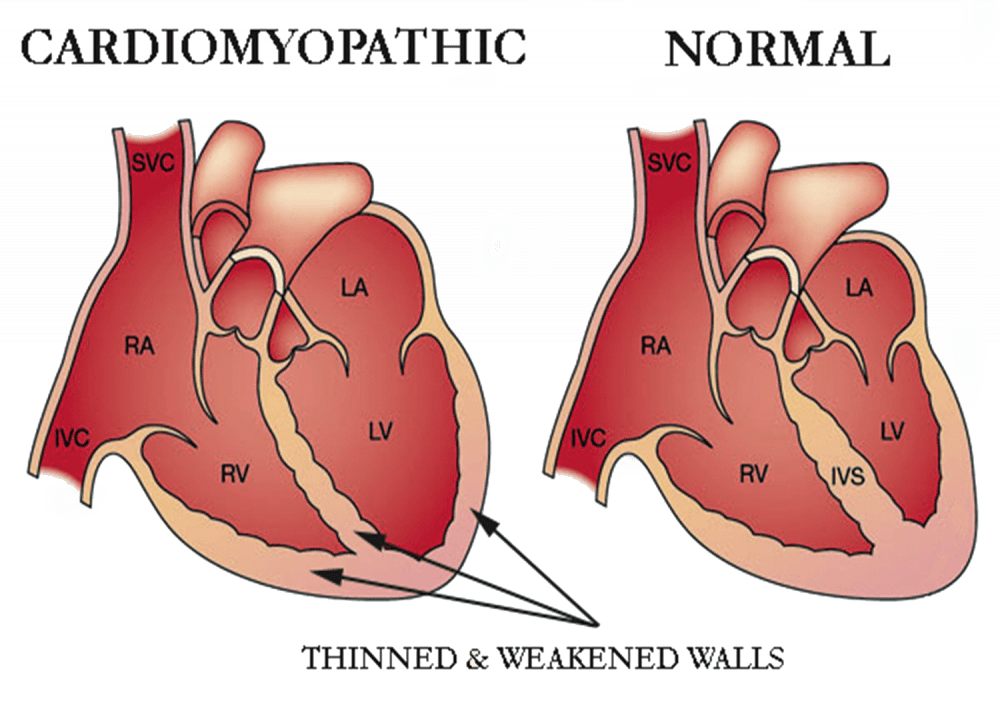
Familial congestive cardiomyopathy, also known as familial dilated cardiomyopathy, is a genetic condition that affects the heart muscle, leading to enlargement and weakening of the heart. Symptoms of familial congestive cardiomyopathy can vary widely among affected individuals and may include:
- Shortness of breath: Especially during physical activity or when lying flat.
- Fatigue: Feeling tired or weak, even with minimal exertion.
- Swelling (edema): Particularly in the legs, ankles, feet, or abdomen, due to fluid retention.
- Palpitations: Sensations of rapid, fluttering, or pounding heartbeats.
- Chest pain or discomfort: Not always present, but can occur, especially with exertion or when lying flat.
- Dizziness or lightheadedness: Especially when standing up quickly.
- Fainting (syncope): Due to reduced blood flow to the brain.
- Decreased exercise tolerance: Feeling unable to exercise as much as usual.
It’s important to note that some individuals with familial congestive cardiomyopathy may not have any symptoms, especially in the early stages of the condition. Symptoms can worsen over time as the heart becomes less able to pump blood effectively, leading to complications such as heart failure, arrhythmias (abnormal heart rhythms), and blood clots.
If you or a family member have been diagnosed with familial congestive cardiomyopathy or have a family history of the condition, it’s important to seek medical evaluation and monitoring by a healthcare provider to manage symptoms and reduce the risk of complications. Treatment may include medications, lifestyle changes, and in some cases, implantation of a defibrillator or heart transplant.
What are the causes of familial congestive cardiomyopathy?
Familial congestive cardiomyopathy, also known as familial dilated cardiomyopathy, is a genetic condition that is inherited in an autosomal dominant pattern, meaning that a person only needs to inherit one copy of the mutated gene from one parent to develop the condition. The exact cause of familial congestive cardiomyopathy is not fully understood, but it is believed to be caused by mutations in certain genes that are involved in the structure and function of the heart muscle.
Several genes have been associated with familial congestive cardiomyopathy, including:
- MYH7: Mutations in the MYH7 gene, which encodes a protein called beta-myosin heavy chain, are associated with familial dilated cardiomyopathy.
- TNNT2: Mutations in the TNNT2 gene, which encodes a protein called cardiac troponin T, have also been linked to familial dilated cardiomyopathy.
- LMNA: Mutations in the LMNA gene, which encodes a protein called lamin A/C, have been associated with dilated cardiomyopathy with conduction system disease.
- TTN: Mutations in the TTN gene, which encodes a protein called titin, have been found in some cases of familial dilated cardiomyopathy.
These genetic mutations can lead to abnormalities in the structure and function of the heart muscle, leading to enlargement and weakening of the heart. Familial congestive cardiomyopathy is a heterogeneous condition, meaning that there may be other genetic and environmental factors that contribute to its development.
It’s important to note that not all individuals with a mutation in a gene associated with familial congestive cardiomyopathy will develop the condition, and the severity of symptoms can vary widely among affected individuals. Genetic counseling is recommended for individuals with a family history of familial congestive cardiomyopathy or who are concerned about their risk of inheriting the condition.
What is the treatment for familial congestive cardiomyopathy?
The treatment for familial congestive cardiomyopathy, also known as familial dilated cardiomyopathy, focuses on managing symptoms, improving heart function, and reducing the risk of complications. Treatment may include:
- Medications: Medications may be prescribed to help the heart pump more effectively, control blood pressure, and manage symptoms such as fluid retention and arrhythmias (abnormal heart rhythms). Common medications include ACE inhibitors, beta-blockers, diuretics, and anticoagulants.
- Lifestyle modifications: Adopting a heart-healthy lifestyle can help manage familial congestive cardiomyopathy. This may include maintaining a healthy diet low in sodium and saturated fats, exercising regularly, maintaining a healthy weight, avoiding tobacco smoke, and limiting alcohol intake.
- Implantable devices: In some cases, implantable devices such as pacemakers or implantable cardioverter-defibrillators (ICDs) may be recommended to help regulate the heart’s rhythm and prevent sudden cardiac arrest.
- Surgical procedures: In severe cases of familial congestive cardiomyopathy, heart transplant surgery may be considered. This involves replacing the diseased heart with a healthy heart from a donor.
- Genetic counseling: Genetic counseling may be recommended for individuals with familial dilated cardiomyopathy and their families to discuss the genetic basis of the condition, inheritance patterns, and options for testing and management.
- Regular monitoring: Regular follow-up visits with a healthcare provider are important to monitor heart function, manage medications, and adjust treatment as needed.
The specific treatment plan for familial congestive cardiomyopathy will depend on the individual’s symptoms, the underlying cause of the condition, and other factors. It’s important for individuals with familial dilated cardiomyopathy to work closely with a healthcare team experienced in managing the condition to develop a personalized treatment plan.