Fibrous Interstitial Pneumonia: Symptoms, Causes, Treatment
What are the symptoms of fibrous interstitial pneumonia?
Fibrosing interstitial pneumonia, also known as idiopathic pulmonary fibrosis (IPF), is a type of interstitial lung disease characterized by progressive scarring of the lung tissue. The symptoms of fibrosing interstitial pneumonia can vary from person to person, but common symptoms may include:
- Shortness of breath: Gradually worsening shortness of breath, especially during physical activity.
- Persistent dry cough: A cough that does not produce phlegm or mucus, which can be persistent and may worsen over time.
- Fatigue: Feeling tired or lacking energy, which can be related to the increased effort required to breathe.
- Weakness: Muscle weakness, which can be related to decreased oxygen levels in the blood.
- Unexplained weight loss: Losing weight without trying, which can be a result of the increased energy expenditure required for breathing.
- Clubbing: Clubbing is a condition in which the fingers and toes become enlarged and rounded at the tips. It is a sign of decreased oxygen in the blood and can occur in advanced stages of fibrosing interstitial pneumonia.
- Cyanosis: Cyanosis is a bluish discoloration of the skin, lips, or nails, which can occur when oxygen levels in the blood are low.
- Chest discomfort: Some people with fibrosing interstitial pneumonia may experience chest discomfort or pain, which can be due to the strain on the lungs caused by the scarring.
- Respiratory failure: In advanced stages of the disease, fibrosing interstitial pneumonia can lead to respiratory failure, where the lungs are no longer able to provide enough oxygen to the body.
It’s important to note that the symptoms of fibrosing interstitial pneumonia can be similar to those of other lung conditions, so a thorough evaluation by a healthcare provider is necessary for an accurate diagnosis. Early diagnosis and management of fibrosing interstitial pneumonia are important for slowing disease progression and improving quality of life.
What are the causes of fibrous interstitial pneumonia?
Fibrosing interstitial pneumonia, or idiopathic pulmonary fibrosis (IPF), is a type of interstitial lung disease in which the cause is unknown. However, several factors are believed to contribute to the development of IPF:
- Genetics: There is evidence to suggest that genetics may play a role in the development of IPF. Some cases of IPF are believed to be familial, meaning they occur in families, suggesting a genetic predisposition to the disease.
- Age: IPF is more common in older adults, particularly those over the age of 50. The risk of developing IPF increases with age.
- Environmental factors: Exposure to certain environmental factors, such as occupational or environmental pollutants, may increase the risk of developing IPF. Cigarette smoking is also a known risk factor for IPF.
- Gastroesophageal reflux disease (GERD): Some studies have suggested a link between GERD and IPF, although the exact nature of this relationship is not fully understood.
- Viral infections: Some viral infections, such as Epstein-Barr virus (EBV) or hepatitis C virus (HCV), have been associated with an increased risk of developing IPF.
- Microscopic injury to the lung: It is believed that repeated micro-injuries to the lung tissue, possibly caused by the inhalation of environmental pollutants or other factors, may lead to the development of IPF.
- Abnormal wound healing: In people with IPF, it is believed that the normal process of wound healing in the lung tissue becomes dysregulated, leading to excessive scarring (fibrosis).
While these factors may contribute to the development of IPF, the exact cause of the disease is not well understood. IPF is a complex condition with likely multiple contributing factors, and more research is needed to fully understand its underlying causes.
What is the treatment for fibrous interstitial pneumonia?
The treatment for fibrosing interstitial pneumonia, or idiopathic pulmonary fibrosis (IPF), aims to slow the progression of the disease, relieve symptoms, and improve quality of life. Treatment options may include:
- Medications:
- Pirfenidone (Esbriet): Pirfenidone is an anti-fibrotic medication that can help slow the progression of IPF and reduce the decline in lung function.
- Nintedanib (Ofev): Nintedanib is another anti-fibrotic medication that can help slow the progression of IPF by reducing the activity of certain growth factors involved in fibrosis.
- Oxygen therapy: Supplemental oxygen therapy can help improve oxygen levels in the blood and relieve symptoms of shortness of breath.
- Pulmonary rehabilitation: Pulmonary rehabilitation programs can help improve exercise tolerance, reduce breathlessness, and improve overall quality of life for people with IPF.
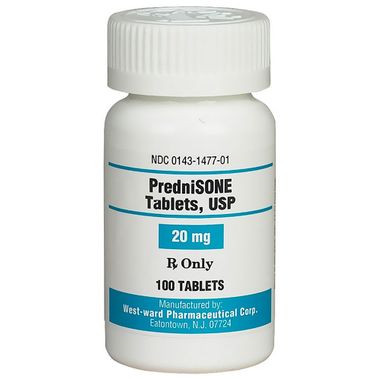
- Corticosteroids: In some cases, corticosteroids such as prednisone may be prescribed to reduce inflammation in the lungs, although their effectiveness in IPF is limited and they are not recommended as a long-term treatment.
- Antifibrotic agents: Some medications that are used to treat other conditions, such as rheumatoid arthritis or cancer, may be used off-label to treat IPF. Examples include azathioprine, cyclophosphamide, and mycophenolate mofetil.
- Lung transplant: In severe cases of IPF where other treatments have not been effective, a lung transplant may be considered. Lung transplantation can improve quality of life and prolong survival in selected patients with IPF.
- Supportive care: Supportive care measures, such as pulmonary rehabilitation, nutritional support, and counseling, can help improve quality of life for people with IPF.
It’s important for individuals with IPF to work closely with a healthcare provider experienced in managing the condition to develop a personalized treatment plan. Early diagnosis and treatment of IPF are important for slowing disease progression and improving outcomes.