Hiatal Hernia: Symptoms, Causes, Treatment
What are the symptoms of a hiatal hernia?
A hiatal hernia occurs when part of the stomach pushes up through the diaphragm and into the chest cavity. This condition can cause a variety of symptoms, including:
- Heartburn: This is the most common symptom of a hiatal hernia. It is a burning sensation in the chest, often after eating, and may be worse when lying down or bending over.
- Regurgitation: Some people with a hiatal hernia may experience a sour or bitter taste in the mouth, especially when lying down or bending over.
- Difficulty swallowing: This symptom, also known as dysphagia, can occur when the hernia compresses the esophagus, making it harder for food to pass through.
- Chest pain: Chest pain associated with a hiatal hernia can mimic the symptoms of a heart attack, although it is typically not as severe. It may be confused with heartburn or indigestion.
- Belching or burping: Excessive belching or burping can be a symptom of a hiatal hernia, especially after eating or drinking.
- Feeling full quickly: Some people with a hiatal hernia may feel full soon after eating, even if they have not eaten much.
- Fatigue: Chronic fatigue may occur due to the discomfort and disruption of normal eating patterns caused by a hiatal hernia.
It’s important to note that not everyone with a hiatal hernia will experience symptoms. In some cases, the condition may be discovered incidentally during imaging tests for other reasons. If you experience persistent or severe symptoms of a hiatal hernia, it’s important to see a healthcare provider for an accurate diagnosis and appropriate treatment.
What are the causes of a hiatal hernia?
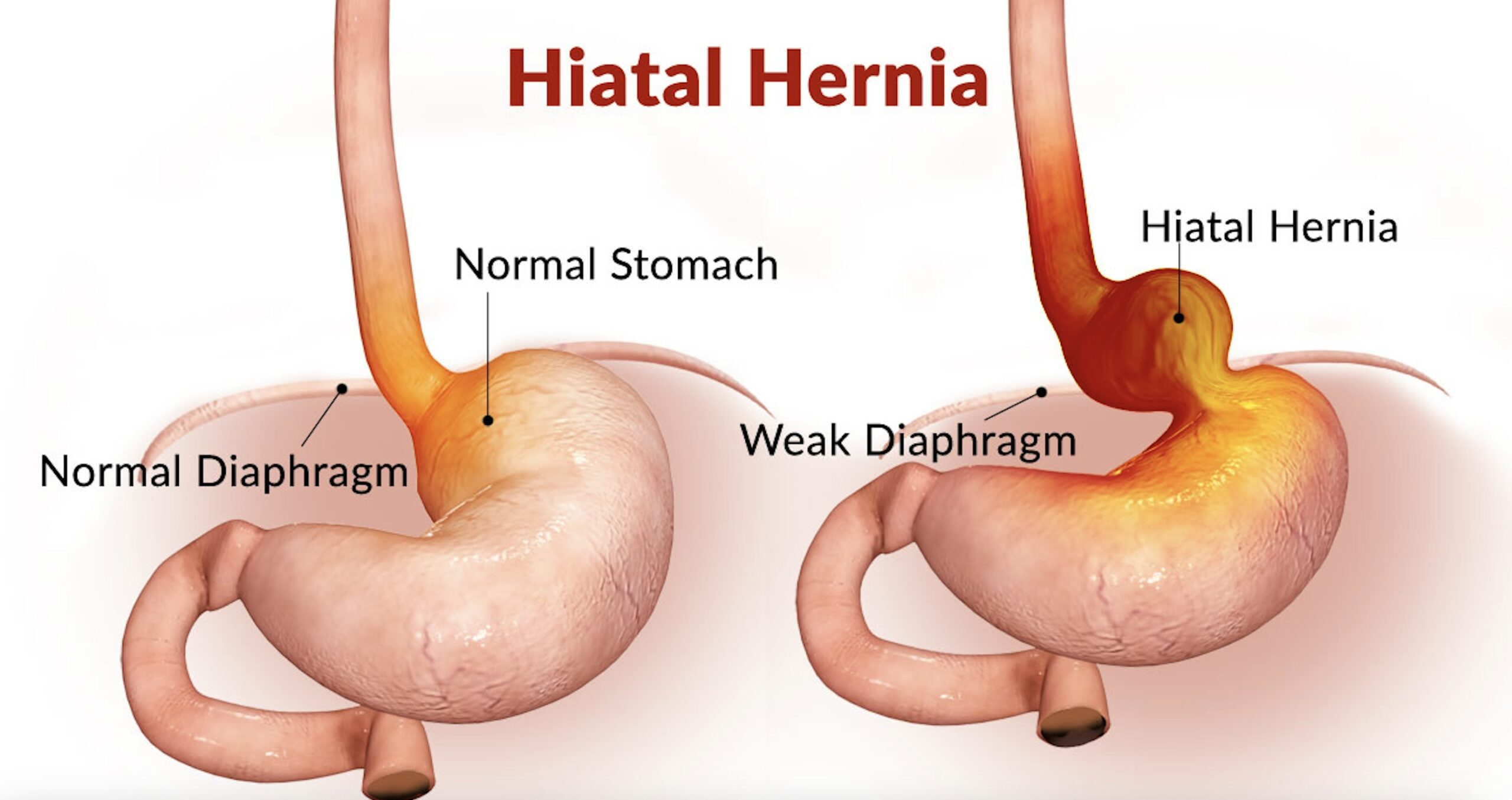
A hiatal hernia occurs when the upper part of the stomach pushes up through the diaphragm into the chest cavity. The exact cause of a hiatal hernia is not always clear, but several factors may contribute to its development, including:
- Weakness in the diaphragm: The diaphragm is a large muscle that separates the chest cavity from the abdomen and helps with breathing. Weakness in the diaphragm can allow the stomach to bulge upward into the chest cavity, leading to a hiatal hernia.
- Age-related changes: As people age, the muscles and tissues that support the diaphragm may weaken, increasing the risk of developing a hiatal hernia.
- Injury or trauma: Injuries to the chest or abdomen, such as from a severe coughing episode, vomiting, or childbirth, can contribute to the development of a hiatal hernia.
- Increased pressure in the abdomen: Conditions or activities that increase pressure in the abdomen, such as obesity, pregnancy, heavy lifting, or straining during bowel movements, can also contribute to the development of a hiatal hernia.
- Genetics: Some people may inherit a predisposition to developing a hiatal hernia, although the specific genetic factors are not well understood.
- Certain health conditions: Conditions that can weaken or damage the muscles and tissues of the diaphragm, such as persistent coughing, chronic obstructive pulmonary disease (COPD), or connective tissue disorders, may increase the risk of developing a hiatal hernia.
It’s important to note that while these factors may increase the risk of developing a hiatal hernia, not everyone with these risk factors will develop the condition. Additionally, some people may develop a hiatal hernia without any identifiable cause.
What is the treatment for a hiatal hernia?
Treatment for a hiatal hernia depends on the severity of symptoms and the presence of complications. In many cases, lifestyle changes and medications can help manage symptoms. However, if symptoms are severe or complications occur, surgery may be necessary. Here are some common treatment options:
- Lifestyle changes:
- Avoiding large meals and eating smaller, more frequent meals
- Avoiding lying down or bending over after eating
- Elevating the head of the bed by 6 to 8 inches
- Losing weight if overweight or obese
- Quitting smoking
- Medications:
- Antacids to neutralize stomach acid
- H2-receptor antagonists or proton pump inhibitors to reduce stomach acid production
- Prokinetic agents to help the stomach empty more quickly
- Surgery:
- If lifestyle changes and medications do not provide relief, or if there are complications such as severe reflux, bleeding, or narrowing of the esophagus, surgery may be recommended.
- The most common surgical procedure for a hiatal hernia is called a Nissen fundoplication, where the upper part of the stomach is wrapped around the lower esophagus to strengthen the sphincter and prevent acid reflux.
- Treatment of complications:
- If a hiatal hernia causes severe GERD (gastroesophageal reflux disease) or esophagitis (inflammation of the esophagus), additional treatments may be necessary to manage these conditions.
It’s important for individuals with a hiatal hernia to work closely with their healthcare providers to develop a treatment plan that is tailored to their specific needs and addresses their symptoms and any underlying conditions. Regular monitoring and follow-up may be necessary to ensure that the treatment plan is effective.