Histiocytosis X: Symptoms, Causes, Treatment
What are the symptoms of histiocytosis X?
Histiocytosis X, also known as Langerhans cell histiocytosis (LCH), is a rare disorder characterized by an excess of abnormal Langerhans cells in various parts of the body. The symptoms can vary widely depending on the organs involved. Common symptoms include:
- Bone pain: Pain or tenderness in the bones, especially the skull, ribs, spine, and long bones.
- Skin rash: Red, scaly, or flaky skin rash that may be itchy.
- Swollen lymph nodes: Enlarged lymph nodes, especially in the neck, armpits, or groin.
- Fever: Low-grade fever that may persist.
- Weight loss: Unexplained weight loss may occur in some cases.
- Fatigue: Feeling tired or lethargic.
- Breathing problems: If LCH affects the lungs, symptoms may include cough, shortness of breath, and chest pain.
- Diabetes insipidus: This condition, characterized by excessive thirst and urination, can occur if LCH affects the pituitary gland.
- Jaundice: Yellowing of the skin and eyes, which can occur if LCH affects the liver.
- Neurological symptoms: In rare cases, LCH can affect the central nervous system, leading to symptoms such as headaches, seizures, or neurological deficits.
The symptoms of LCH can vary greatly from person to person and depend on the extent and location of the disease. Treatment usually involves a multidisciplinary approach and may include chemotherapy, steroid therapy, and other medications by healthcare providers to control the disease and manage symptoms.
What are the causes of histiocytosis X?
The exact cause of histiocytosis X, or Langerhans cell histiocytosis (LCH), is not well understood. It is believed to result from an overproduction and accumulation of immature Langerhans cells, a type of white blood cell that normally helps the body fight infection. However, in LCH, these cells accumulate and form lesions or tumors in various parts of the body.
Some theories suggest that LCH may be triggered by an abnormal response of the immune system, genetic factors, or exposure to certain environmental substances. However, no single cause has been definitively identified, and more research is needed to fully understand the underlying mechanisms of this condition.
What is the treatment for histiocytosis X?
Treatment for histiocytosis X, or Langerhans cell histiocytosis (LCH), depends on the extent and severity of the disease. In many cases, LCH may resolve on its own without treatment. However, when treatment is necessary, it typically involves a multidisciplinary approach and may include the following:
- Observation: In some cases, especially for single or few lesions that are not causing symptoms, a “watch and wait” approach may be recommended to see if the lesions resolve on their own.
- Medications:
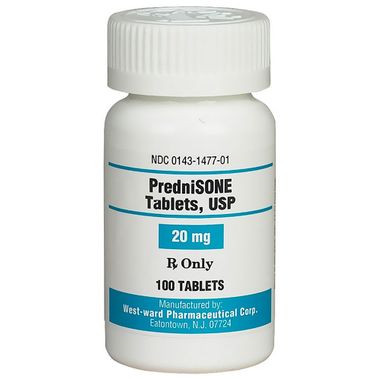
- Steroids: Corticosteroids such as prednisone may be used to reduce inflammation and suppress the immune system.
- Chemotherapy: In more severe cases, chemotherapy drugs such as vinblastine, methotrexate, or cytarabine may be used to kill abnormal cells and prevent them from growing.
- Targeted therapy: Drugs that target specific molecules involved in the growth and survival of Langerhans cells, such as BRAF inhibitors, may be used in some cases.
- Surgery: Surgical removal of lesions may be necessary in certain cases, especially if they are causing significant symptoms or complications.
- Radiation therapy: Radiation therapy may be used to treat lesions that are not responding to other treatments or are causing severe symptoms.
- Bone marrow transplant: In very severe cases or cases that do not respond to other treatments, a bone marrow transplant may be considered to replace damaged bone marrow with healthy stem cells.
The choice of treatment depends on several factors, including the age and overall health of the patient, the extent and location of the disease, and the response to previous treatments. It is important for patients with LCH to be treated by a healthcare team experienced in managing this rare condition.