How do doctors deal with breech birth?
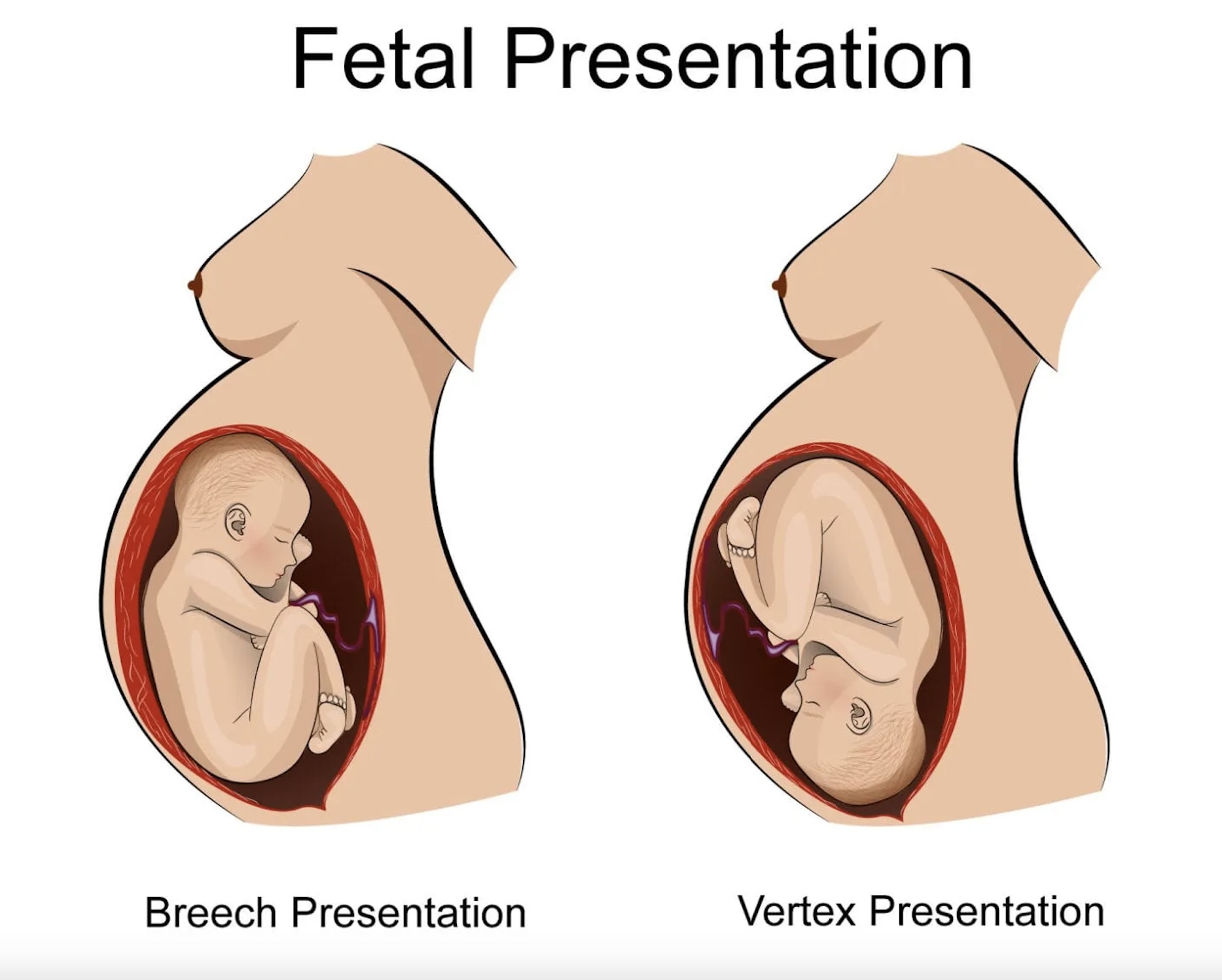
When a baby is in the breech position (buttocks or feet first) near the due date, doctors have a few different options for dealing with it:
- External Cephalic Version (ECV)
- This is an attempt to manually turn the baby into a head-down position through manipulations of the abdomen.
- It is typically tried between 36-38 weeks if the baby is breech.
- Success rates are around 50-60% with experienced providers.
- It carries small risks like placental problems or emergency C-section.
- Planned Cesarean Section
- If ECV is unsuccessful or not possible, a scheduled C-section is often recommended to avoid the risks of a vaginal breech delivery.
- C-sections are considered the safest delivery option for a frank or footling breech baby.
- Vaginal Breech Delivery
- In certain situations, an experienced provider may attempt a vaginal breech delivery.
- This is more common for complete or frank breech position.
- It requires close monitoring and may need interventions like forceps or episiotomy.
- Risks include head entrapment, umbilical cord issues, birth injuries.
- Version with Induction
- In some cases, a doctor may try to turn the baby during early labor, followed by immediate induction if successful.
Factors like the specific breech type, size of baby, pelvis size, placenta location, and provider experience all weigh into the decision.
The trend has shifted toward planned C-sections for breech babies, as it eliminates the risks of ECV and vaginal breech delivery complications. But each case is individualized.
Doctors aim to make the safest choice for both mother and baby based on their specific situation. Early detection and counseling about the options is important.
How common is breech birthing?
Breech birth, where the baby is positioned bottom-first rather than head-first in the womb, occurs in approximately 3-4% of full-term births. However, the frequency of breech presentation can vary depending on several factors, including the gestational age of the baby, the number of pregnancies a woman has had, and whether there are any underlying conditions affecting the uterus or the baby’s position.
Factors Affecting Breech Presentation Frequency:
- Gestational Age: Breech presentation is more common earlier in pregnancy but usually corrects itself as the pregnancy progresses. By the time of delivery, most babies will have turned into a head-down position.
- Multiparity: Women who have had multiple pregnancies may be more likely to experience breech presentation in subsequent pregnancies.
- Uterine Abnormalities: Conditions such as uterine fibroids or abnormalities in the shape of the uterus can affect the baby’s position.
- Polyhydramnios: Excessive amniotic fluid in the uterus may increase the likelihood of breech presentation.
- Fetal Factors: Certain factors related to the baby, such as abnormalities in the shape or size of the fetus, can contribute to breech presentation.
Diagnosis and Management:
- Prenatal Care: Breech presentation is typically diagnosed during routine prenatal exams through palpation of the abdomen or ultrasound imaging.
- External Cephalic Version (ECV): This procedure involves manually attempting to turn the baby into a head-down position from the outside of the mother’s abdomen. ECV is often attempted around 37 weeks of pregnancy if the baby is still breech.
- Vaginal Breech Delivery: In some cases, vaginal delivery of a breech-presenting baby may be considered, especially if certain criteria are met, such as the baby being in a frank breech position and the healthcare provider having expertise in breech delivery.
- Cesarean Section (C-section): Many healthcare providers recommend a planned cesarean delivery for breech-presenting babies due to potential risks associated with vaginal breech delivery, such as head entrapment or umbilical cord compression.
Summary:
Breech presentation occurs in approximately 3-4% of full-term pregnancies. Factors influencing breech presentation include gestational age, multiparity, uterine abnormalities, excessive amniotic fluid, and fetal factors. Diagnosis is typically made during prenatal care, and management options include external cephalic version (ECV), vaginal breech delivery (in select cases), or planned cesarean section. Each case is unique, and decisions regarding delivery method should be made in consultation with healthcare providers based on individual circumstances and preferences.