Hypokalemia: Symptoms, Causes, Treatment
What are the symptoms of hypokalemia?
Hypokalemia is a condition characterized by low levels of potassium in the blood. Symptoms of hypokalemia can vary depending on the severity of the deficiency but may include:
- Weakness: Muscle weakness, especially in the legs, arms, or trunk, is a common symptom of hypokalemia.
- Fatigue: Feeling unusually tired or fatigued, even with normal activity, can be a symptom of hypokalemia.
- Muscle cramps: Cramping or spasms in the muscles, especially in the legs, arms, or abdomen, can occur with hypokalemia.
- Constipation: Hypokalemia can affect the muscles in the digestive tract, leading to constipation.
- Irregular heartbeat: Low potassium levels can affect the heart’s ability to maintain a regular rhythm, leading to palpitations or irregular heartbeats.
- Numbness or tingling: Some people with hypokalemia may experience numbness or tingling, especially in the extremities.
- Increased urination: Hypokalemia can affect the kidneys’ ability to concentrate urine, leading to increased urination and thirst.
- Muscle weakness or paralysis: Severe hypokalemia can lead to muscle weakness or paralysis, which can be life-threatening if it affects the muscles involved in breathing or swallowing.
It’s important to note that some people with mild hypokalemia may not experience any symptoms. However, if you experience any of the above symptoms, especially if they are severe or persistent, it’s important to see a healthcare provider for an evaluation. Hypokalemia can be diagnosed with a simple blood test, and treatment may involve potassium supplements or changes in diet.
What are the causes of hypokalemia?
Hypokalemia, or low potassium levels in the blood, can be caused by a variety of factors. Some common causes of hypokalemia include:
- Diuretics: Diuretics, also known as water pills, are medications that increase the excretion of water and electrolytes, including potassium, from the body. This is a common cause of drug-induced hypokalemia.
- Vomiting and diarrhea: Conditions that cause severe vomiting or diarrhea can lead to the loss of potassium from the body.
- Magnesium deficiency: Magnesium is needed for the body to maintain potassium levels. A deficiency in magnesium can lead to hypokalemia.
- Kidney disease: Conditions that affect the kidneys’ ability to retain potassium, such as kidney disease or renal tubular acidosis, can lead to hypokalemia.
- Excessive sweating: Profuse sweating, such as that seen with intense physical activity or in hot weather, can lead to the loss of potassium from the body.
- Certain medications: In addition to diuretics, other medications can cause hypokalemia, including laxatives, corticosteroids, and some antibiotics.
- Alcoholism: Chronic alcohol abuse can lead to malnutrition and electrolyte imbalances, including hypokalemia.
- Eating disorders: Conditions such as anorexia nervosa or bulimia can lead to malnutrition and electrolyte imbalances, including hypokalemia.
- Hyperaldosteronism: This is a condition characterized by high levels of aldosterone, a hormone that regulates potassium levels. Hyperaldosteronism can lead to the loss of potassium from the body.
- Certain genetic conditions: Some rare genetic conditions, such as Bartter syndrome or Gitelman syndrome, can lead to electrolyte imbalances, including hypokalemia.
It’s important to note that the underlying cause of hypokalemia may need to be identified and treated to prevent recurrence. Treatment for hypokalemia may involve potassium supplements, changes in diet, or treating the underlying medical condition.
What is the treatment for hypokalemia?
The treatment for hypokalemia, or low potassium levels in the blood, depends on the underlying cause and the severity of the deficiency. In mild cases, treatment may involve dietary changes or supplements. In more severe cases, intravenous (IV) potassium may be necessary. Some common treatments for hypokalemia include:
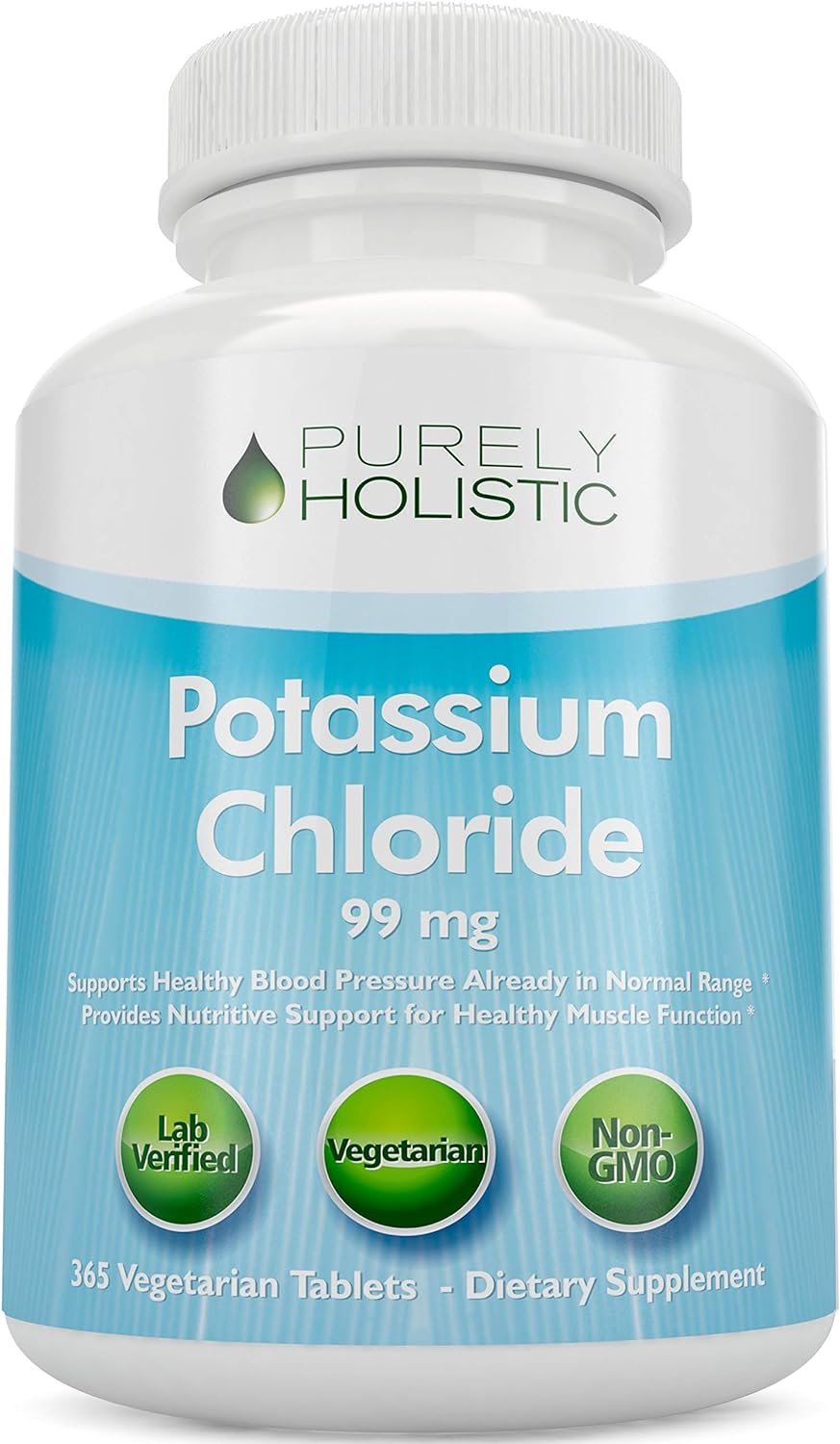
- Potassium supplements: Oral potassium supplements are often used to treat mild to moderate hypokalemia. These supplements come in various forms, including potassium chloride and potassium citrate. It’s important to follow your healthcare provider’s instructions when taking potassium supplements, as too much potassium can be dangerous.
- Dietary changes: Eating potassium-rich foods can help raise potassium levels in the blood. Foods that are high in potassium include bananas, oranges, tomatoes, potatoes, spinach, and beans.
- Intravenous (IV) potassium: In severe cases of hypokalemia, or if the person cannot take oral supplements, potassium may be given intravenously. This is usually done in a hospital setting under close supervision.
- Treating the underlying cause: In addition to replacing potassium, it’s important to identify and treat the underlying cause of hypokalemia. This may involve adjusting medications, treating kidney disease or other medical conditions, or addressing lifestyle factors such as excessive sweating or alcohol abuse.
- Monitoring: Regular monitoring of potassium levels is important to ensure that treatment is effective and to prevent recurrence of hypokalemia.
It’s important to note that potassium supplements should only be taken under the supervision of a healthcare provider, as too much potassium can be harmful. It’s also important to follow any dietary recommendations provided by your healthcare provider to help maintain normal potassium levels.