Hypoplastic Left Heart Syndrome (HLHS): Symptoms, Causes, Treatment
What are the symptoms of HLHS?
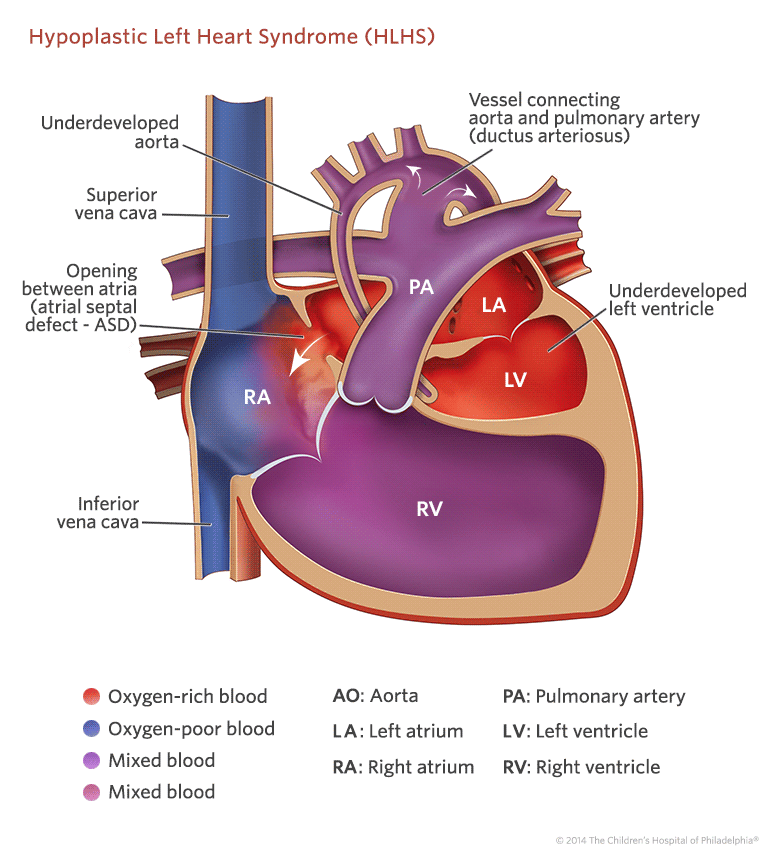
Hypoplastic left heart syndrome (HLHS) is a complex and serious congenital heart defect where the left side of the heart is severely underdeveloped. Symptoms of HLHS typically present shortly after birth and can include:
- Cyanosis: Bluish discoloration of the skin, lips, and nails due to reduced oxygen levels in the blood.
- Rapid or difficulty breathing: The baby may breathe rapidly or have trouble breathing, especially during feeding or crying.
- Poor feeding: The baby may have difficulty feeding and may tire easily during feeding.
- Cold hands and feet: Due to poor circulation.
- Weak pulse: The pulse may be weak or difficult to detect.
- Lethargy: The baby may appear unusually tired or inactive.
- Heart murmur: A heart murmur, which is an abnormal sound heard during a heartbeat, may be present.
- Heart failure: In severe cases, heart failure can occur, leading to symptoms such as swelling of the feet, ankles, or abdomen; rapid weight gain; and difficulty breathing, especially when lying flat.
- Shock: In some cases, HLHS can lead to shock, a life-threatening condition where the body’s organs do not receive enough blood flow.
It’s important to note that the symptoms of HLHS can vary depending on the severity of the condition and other factors. Babies born with HLHS require immediate medical attention and often require surgery or other interventions to improve blood flow and heart function.
What are the causes of HLHS?
Hypoplastic left heart syndrome (HLHS) is a congenital heart defect, meaning it is present at birth. The exact cause of HLHS is not known, but it is believed to result from a combination of genetic and environmental factors. Some factors that may contribute to the development of HLHS include:
- Genetic factors: There is evidence to suggest that HLHS may have a genetic component, as it can sometimes occur in families with a history of congenital heart defects. However, the specific genes involved in HLHS are not yet fully understood.
- Environmental factors: Exposure to certain substances or conditions during pregnancy may increase the risk of HLHS. These factors may include maternal diabetes, certain medications taken during pregnancy, or exposure to toxins or infections.
- Chromosomal abnormalities: HLHS is sometimes associated with certain chromosomal abnormalities, such as Turner syndrome or trisomy 13.
- Other heart defects: Some cases of HLHS may be associated with other heart defects, suggesting that there may be a complex interplay of factors that contribute to the development of the condition.
It’s important to note that while these factors may increase the risk of HLHS, the majority of cases occur sporadically, meaning they occur without a known genetic or environmental cause. More research is needed to fully understand the causes of HLHS and how it develops. If you suspect HLHS, it is important to seek help from a healthcare provider.
What is the treatment for HLHS?
The treatment for hypoplastic left heart syndrome (HLHS) typically involves a series of surgeries and other interventions aimed at improving the function of the heart and circulation. The specific treatment plan may vary depending on the individual case and the severity of the condition, but it often includes the following:
- Medications: Infants with HLHS may be given medications to help the heart function more efficiently and to manage symptoms such as fluid retention or irregular heart rhythms.
- Surgery: The main treatment for HLHS is a series of surgeries known as the Norwood procedure, the Glenn procedure, and the Fontan procedure. These surgeries are typically performed in stages, with the first stage (Norwood procedure) usually done within the first week of life. These surgeries are complex and aim to reroute blood flow through the heart and improve circulation.
- Heart transplant: In some cases, a heart transplant may be considered if the child’s heart cannot be adequately repaired with surgery.
- Ongoing care: Children with HLHS require ongoing monitoring and care by a team of specialists, including pediatric cardiologists, cardiac surgeons, and other healthcare providers. They may also require regular check-ups, medications, and lifestyle modifications to manage their condition.
- Supportive therapies: Depending on the child’s needs, other supportive therapies such as physical therapy, occupational therapy, and speech therapy may be recommended to help improve their quality of life.
The treatment of HLHS is complex and requires a multidisciplinary approach. The goal of treatment is to improve the child’s heart function, relieve symptoms, and improve their overall quality of life. Early diagnosis and treatment are key to achieving the best outcomes for children with HLHS.