Idiopathic Pulmonary Fibrosis: Symptoms, Causes, Treatment
What are the symptoms of idiopathic pulmonary fibrosis?
Idiopathic pulmonary fibrosis (IPF) is a chronic and progressive lung disease characterized by scarring of the lung tissue. The symptoms of IPF can vary from person to person, but common symptoms may include:
- Shortness of breath (dyspnea): This is often the main symptom of IPF and tends to worsen over time, especially with physical activity.
- Persistent dry cough: A cough that does not produce phlegm (mucus) is common in IPF. The cough may be mild at first but can become more frequent and bothersome as the disease progresses.
- Fatigue: Feeling tired or fatigued, even after rest or with minimal exertion, is common in IPF.
- Weakness: Some people with IPF may experience weakness or a general feeling of being unwell.
- Clubbing: Clubbing is a condition where the fingers and toes become enlarged and the nails curve around the fingertips. It can be a sign of advanced IPF.
- Weight loss: Some people with IPF may experience unintentional weight loss, often due to a reduced appetite.
- Muscle and joint pain: Pain in the muscles or joints is possible, although less common than other symptoms.
The symptoms of IPF can be similar to those of other lung diseases, making it challenging to diagnose. If you experience any of these symptoms, especially if they persist or worsen over time, it’s important to see a healthcare provider for an evaluation. Early diagnosis and treatment can help slow the progression of IPF and improve quality of life.
What are the causes of idiopathic pulmonary fibrosis?
The exact cause of idiopathic pulmonary fibrosis (IPF) is unknown, hence the term “idiopathic,” which means of unknown cause. However, several factors and mechanisms are believed to contribute to the development of IPF:
- Genetics: There appears to be a genetic predisposition to IPF, as the disease can run in families. Mutations in certain genes, such as the surfactant protein C (SFTPC) gene, have been linked to an increased risk of developing IPF.
- Age: IPF is more common in older adults, with most cases diagnosed in individuals over the age of 50.
- Environmental exposures: Chronic exposure to certain environmental factors, such as dust, fumes, pollutants, and possibly viral infections, may play a role in the development of IPF.
- Abnormal wound healing: It is believed that repeated injury to the lung tissue leads to abnormal wound healing, which results in the formation of scar tissue (fibrosis) in the lungs.
- Immune system dysfunction: Dysfunction of the immune system may contribute to the development of IPF, although the exact mechanisms are not fully understood.
- Other risk factors: Smoking, gastroesophageal reflux disease (GERD), and certain occupations that involve exposure to dust or pollutants may also increase the risk of developing IPF.
It’s important to note that while these factors may contribute to the development of IPF, the exact cause of the disease remains unknown in most cases. Ongoing research is focused on understanding the underlying mechanisms of IPF and developing more effective treatments.
What is the treatment for idiopathic pulmonary fibrosis?
The treatment for idiopathic pulmonary fibrosis (IPF) aims to slow the progression of the disease, relieve symptoms, improve quality of life, and prolong survival. Treatment approaches may include:
- Medications:
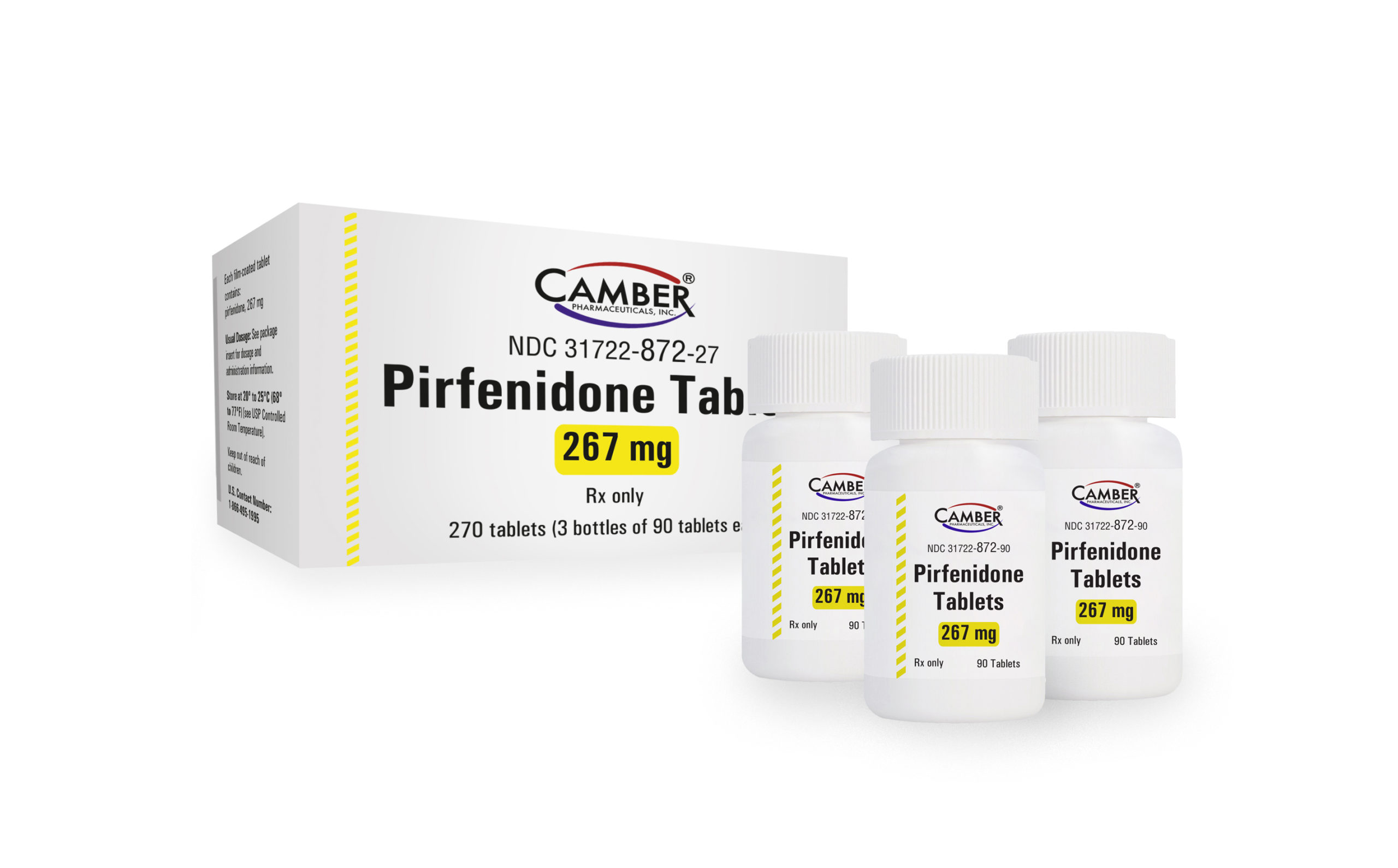
- Pirfenidone and nintedanib: These are two medications approved for the treatment of IPF. They can help slow the progression of the disease and improve lung function in some people.
- Corticosteroids: While corticosteroids were previously used to treat IPF, they are no longer recommended as they have not been shown to be effective and may have harmful side effects.
- Oxygen therapy: Supplemental oxygen therapy can help improve oxygen levels in the blood and reduce shortness of breath.
- Pulmonary rehabilitation: Pulmonary rehabilitation programs can help improve lung function, reduce symptoms, and improve quality of life through exercise, education, and support.
- Lung transplant: For some people with advanced IPF, lung transplantation may be an option. Lung transplantation can improve quality of life and prolong survival in carefully selected candidates.
- Supportive care: This may include symptom management, such as cough suppressants or bronchodilators, and measures to prevent and treat complications such as infections or pulmonary hypertension.
- Clinical trials: Participation in clinical trials may be considered to explore new treatment options and contribute to the advancement of knowledge about IPF.
It’s important for individuals with IPF to work closely with a healthcare team experienced in managing the condition to develop a personalized treatment plan. Regular monitoring and follow-up are essential to monitor disease progression, adjust treatment as needed, and address any complications or changes in symptoms.