Idiopathic Thrombocytopenic Purpura: Symptoms, Causes, Treatment
What are the symptoms of idiopathic thrombocytopenic purpura?
Idiopathic thrombocytopenic purpura (ITP) is a disorder that can lead to easy or excessive bruising and bleeding due to a low platelet count. The symptoms of ITP can vary widely among individuals and may include:
- Petechiae: Small, flat, red or purple spots on the skin caused by bleeding under the skin. These spots are often found on the lower legs but can occur anywhere on the body.
- Purpura: Larger, bruise-like areas of skin discoloration caused by bleeding under the skin. Purpura may appear as red or purple blotches and can vary in size.
- Easy bruising: People with ITP may bruise easily, even from minor bumps or injuries. The bruises may be larger or more numerous than expected.
- Bleeding: In more severe cases of ITP, bleeding may occur from the gums, nose, or digestive tract. Women may experience heavy menstrual bleeding.
- Blood in urine or stool: In rare cases, ITP can cause bleeding in the urinary or gastrointestinal tract, leading to blood in the urine or stool.
- Fatigue: Some people with ITP may experience fatigue or weakness, though this is a less specific symptom that can occur in many conditions.
It’s important to note that the severity and frequency of symptoms can vary greatly among individuals with ITP. Some people may have mild symptoms or periods of remission, while others may have more severe and persistent symptoms. If you experience any of these symptoms, especially if they are persistent or severe, it’s important to see a healthcare provider for evaluation and diagnosis.
What are the causes of idiopathic thrombocytopenic purpura?
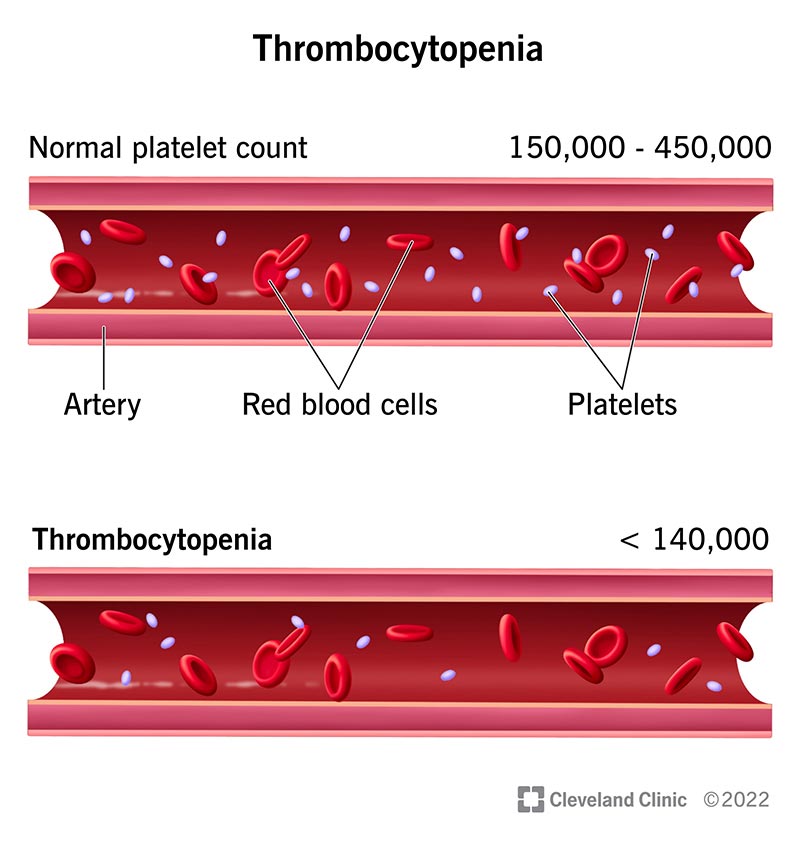
The exact cause of idiopathic thrombocytopenic purpura (ITP) is not fully understood. However, it is believed to be an autoimmune disorder, where the immune system mistakenly attacks and destroys platelets in the blood. Platelets are cells that help the blood clot, and a low platelet count can lead to easy or excessive bruising and bleeding.
In some cases, ITP may occur after a viral infection, such as the flu, or as a complication of another autoimmune disorder, such as lupus. However, in many cases, the cause of ITP is unknown, which is why it is called “idiopathic.”
Other factors that may contribute to the development of ITP include:
- Genetic predisposition: There may be a genetic component to ITP, as it sometimes occurs in families.
- Environmental factors: Certain environmental factors, such as exposure to certain medications, chemicals, or infections, may trigger the immune system to attack platelets in susceptible individuals.
- Immune system dysfunction: Dysfunction in the immune system, such as an imbalance in immune cell populations or an overactive immune response, may play a role in the development of ITP.
- Hormonal factors: ITP is more common in women than in men, and hormonal factors may contribute to its development. For example, ITP may occur during pregnancy or in women who have recently given birth.
- Chronic conditions: Some chronic conditions, such as certain infections, inflammatory disorders, or cancers, may be associated with an increased risk of developing ITP.
It’s important to note that while these factors may contribute to the development of ITP, the condition is considered idiopathic in most cases, meaning that the specific cause is unknown. Treatment for ITP aims to increase the platelet count and prevent bleeding complications, and may include medications, such as corticosteroids or immune-suppressing drugs, and in some cases, surgery to remove the spleen.
What is the treatment for idiopathic thrombocytopenic purpura?
The treatment for idiopathic thrombocytopenic purpura (ITP) depends on the severity of the condition and the risk of bleeding. In some cases, treatment may not be necessary, especially if the platelet count is only mildly low and there are no signs of bleeding. However, if treatment is needed, it may include:
- Corticosteroids: Drugs such as prednisone or dexamethasone may be used to suppress the immune system and reduce the destruction of platelets.
- Intravenous immunoglobulin (IVIG): This treatment involves infusions of immunoglobulin, which can help increase the platelet count by blocking the antibodies that are attacking the platelets.
- Anti-D immunoglobulin: This treatment is specifically used for people with Rh-positive blood who have not responded to other treatments. It works by binding to red blood cells and preventing the immune system from attacking platelets.
- Immune-suppressing drugs: Drugs such as rituximab, azathioprine, or mycophenolate mofetil may be used to suppress the immune system and reduce platelet destruction.
- Splenectomy: In severe cases of ITP that do not respond to other treatments, surgical removal of the spleen (splenectomy) may be recommended. The spleen is where many platelets are destroyed, so removing it can help increase the platelet count.
- Thrombopoietin receptor agonists: Drugs such as eltrombopag and romiplostim can stimulate the production of platelets in the bone marrow and are used for people who have not responded to other treatments.
- Platelet transfusions: In cases of severe bleeding or very low platelet counts, platelet transfusions may be necessary to prevent or treat bleeding episodes. However, these are usually reserved for emergency situations due to the risk of complications.
Treatment for ITP is often individualized based on the patient’s specific situation, including the severity of the condition, the presence of bleeding, and the response to previous treatments. It’s important for individuals with ITP to work closely with their healthcare providers to develop a treatment plan that is right for them.