Impetigo: Symptoms, Causes, Treatments
What are the symptoms of impetigo?
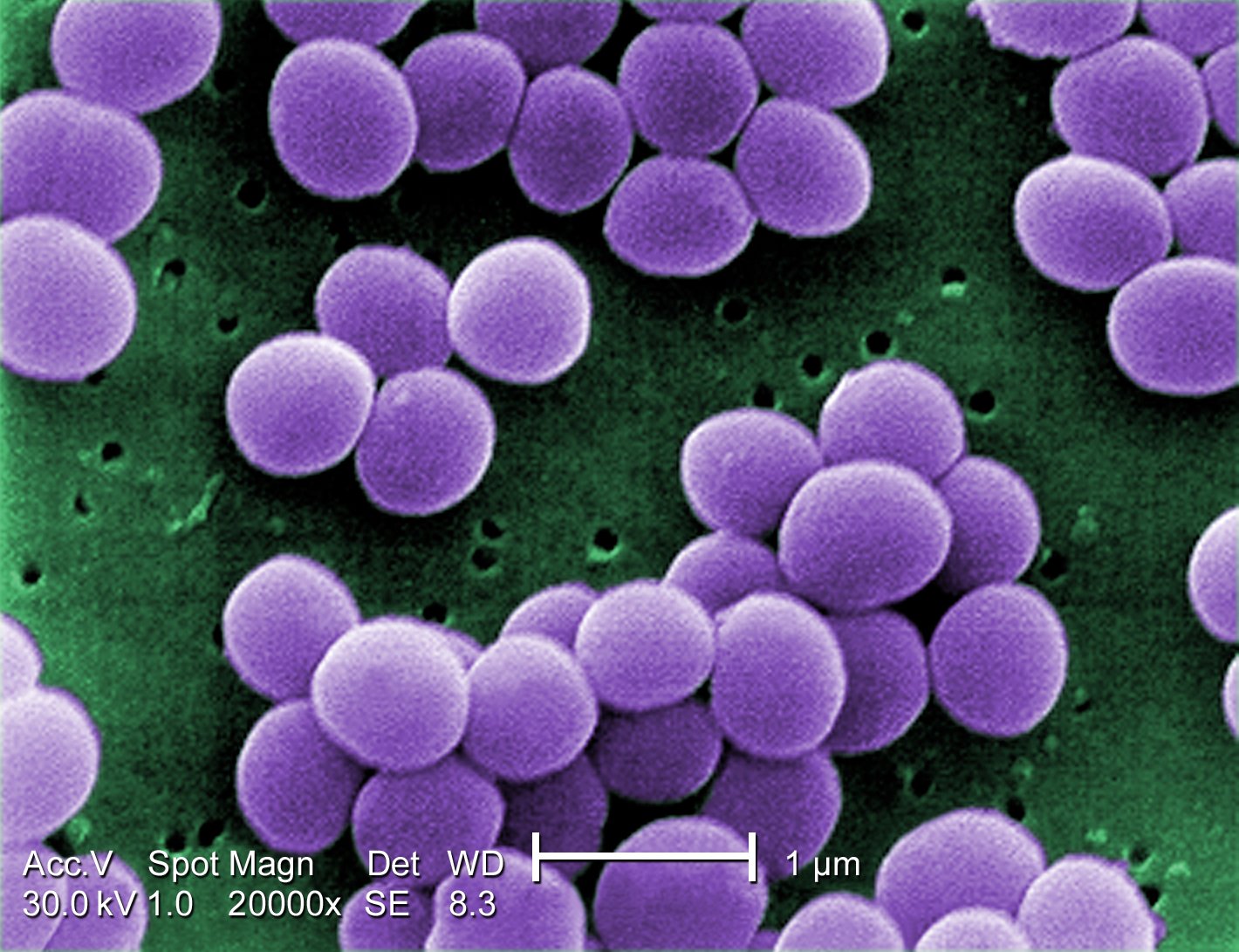
Impetigo is a highly contagious skin infection caused by bacteria, most commonly Staphylococcus aureus or Streptococcus pyogenes. The symptoms of impetigo can vary depending on the type of impetigo (bullous or non-bullous) and the severity of the infection. Common symptoms of impetigo may include:
- Red sores: The most characteristic symptom of impetigo is the presence of red sores that quickly rupture and ooze fluid, forming a yellowish-brown crust. These sores can occur anywhere on the body but are most commonly found around the mouth and nose.
- Itching: The affected area may be itchy, and scratching can spread the infection to other parts of the body.
- Pain: The sores may be painful, especially if they are large or located in areas where there is friction or pressure.
- Swollen lymph nodes: In some cases, nearby lymph nodes may become swollen and tender.
- Fever: In more severe cases of impetigo, particularly if the infection has spread beyond the skin, fever may occur.
It’s important to note that impetigo is most common in children, particularly those between the ages of 2 and 5, but it can occur in people of any age. Impetigo is usually not serious and can be treated with antibiotics. However, if left untreated, impetigo can lead to complications such as cellulitis (a deeper skin infection), scarring, or kidney problems (in cases of streptococcal impetigo). If you suspect you or your child has impetigo, it’s important to see a healthcare provider for proper diagnosis and treatment.
What are the causes of impetigo?
Impetigo is caused by bacterial infection, most commonly by Staphylococcus aureus or Streptococcus pyogenes (also known as group A Streptococcus). These bacteria can enter the skin through cuts, scrapes, insect bites, or other breaks in the skin, leading to infection. Impetigo is highly contagious and can spread through direct contact with an infected person or contaminated objects, such as towels, clothing, or bedding.
Risk factors for impetigo include:
1. Age: Impetigo is most common in children, particularly those between the ages of 2 and 5.
2. Warm, humid weather: Impetigo is more common in warm, humid climates.
3. Crowded or unsanitary living conditions: Impetigo is more likely to occur in settings where there is close contact between individuals, such as schools, daycare centers, and prisons.
4. Skin conditions: People with existing skin conditions, such as eczema, dermatitis, or insect bites, may be more prone to developing impetigo.
5. Compromised immune system: People with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy, are at higher risk of developing impetigo.
6. Injury to the skin: Any break in the skin, such as a cut, scrape, or insect bite, can provide an entry point for bacteria.
It’s important to practice good hygiene, including regular handwashing, to help prevent the spread of impetigo. Prompt treatment with antibiotics is usually effective in clearing the infection and reducing the risk of complications. If you suspect you or your child has impetigo, it’s important to see a healthcare provider for proper diagnosis and treatment.
What is the treatment for impetigo?
The treatment for impetigo typically involves topical or oral antibiotics to eliminate the bacteria causing the infection. The choice of treatment depends on the severity of the infection and the type of impetigo (bullous or non-bullous). Common treatment options for impetigo may include:
- Topical antibiotics: For mild cases of impetigo, topical antibiotics in the form of ointments or creams may be prescribed. These medications are applied directly to the affected areas of the skin.
- Oral antibiotics: For more severe or widespread cases of impetigo, or for cases that do not respond to topical treatment, oral antibiotics may be prescribed. These medications are taken by mouth and work to eliminate the bacteria causing the infection.
- Cleaning the affected area: It is important to keep the affected area clean and dry. Gently wash the affected area with soap and water, and then apply the prescribed antibiotic ointment or cream as directed.
- Avoiding scratching: It is important to avoid scratching or picking at the sores, as this can spread the infection and delay healing.
- Covering the sores: If the impetigo is oozing or crusted, covering the sores with a clean bandage can help prevent the spread of bacteria to others.
- Good hygiene: Practicing good hygiene, such as washing your hands regularly and avoiding sharing personal items like towels and razors, can help prevent the spread of impetigo.
In most cases, impetigo clears up within a few weeks with appropriate treatment. However, it is important to finish the entire course of antibiotics, even if the symptoms improve, to ensure that the infection is completely eliminated. If you or your child has impetigo, it is important to see a healthcare provider for proper diagnosis and treatment.