Lennox-Gastaut Syndrome: Symptoms, Causes, Treatment
What are the symptoms of Lennox-Gastaut syndrome?
Lennox-Gastaut syndrome (LGS) is a rare and severe form of epilepsy that usually begins in early childhood. It is characterized by multiple types of seizures and developmental delays. The symptoms of Lennox-Gastaut syndrome can vary, but they often include:
- Multiple types of seizures: Individuals with LGS typically experience several different types of seizures, including tonic seizures (sudden stiffening of the muscles), atonic seizures (sudden loss of muscle tone), and atypical absence seizures (staring spells with subtle movements).
- Developmental delays: Children with LGS often experience delays in reaching developmental milestones, such as walking and talking.
- Intellectual disability: Many individuals with LGS have intellectual disability, ranging from mild to severe.
- Behavioral problems: Behavioral problems, such as hyperactivity, aggression, or autistic-like behaviors, may be present in some individuals with LGS.
- Distinctive EEG patterns: Electroencephalogram (EEG) testing often shows a characteristic pattern of slow spike-and-wave complexes, which is typical of LGS.
- Sleep disturbances: Individuals with LGS may experience sleep disturbances, including nighttime seizures and disrupted sleep patterns.
- Motor impairments: Some individuals with LGS may have difficulties with coordination and motor skills.
- Behavioral and emotional difficulties: Behavioral and emotional problems, such as mood swings, anxiety, or depression, may occur in individuals with LGS.
- Autonomic dysfunction: Some individuals with LGS may experience autonomic dysfunction, which can manifest as changes in heart rate, blood pressure, or temperature regulation.
- Growth disturbances: Children with LGS may experience growth disturbances, such as slowed growth or delayed puberty.
- Gastrointestinal problems: Some individuals with LGS may experience gastrointestinal problems, such as constipation or gastroesophageal reflux.
The symptoms of Lennox-Gastaut syndrome can have a significant impact on quality of life and may require a multidisciplinary approach to management, including medications, dietary therapy, and supportive care. Early diagnosis and appropriate treatment are important for managing the symptoms of LGS and improving outcomes, so you should consult a healthcare provider as soon as possible.
What are the causes of Lennox-Gastaut syndrome?
The exact cause of Lennox-Gastaut syndrome (LGS) is often unknown, but it is believed to involve a combination of genetic, structural, and developmental factors. Some of the potential causes and risk factors for LGS include:
- Brain abnormalities: LGS is often associated with structural abnormalities or damage to the brain, such as cortical dysplasia, encephalitis, brain malformations, or brain injuries. These abnormalities can disrupt normal brain function and contribute to the development of seizures and cognitive impairments seen in LGS.
- Genetic factors: In some cases, LGS may have a genetic component. Certain genetic mutations or abnormalities may increase the risk of developing LGS. However, LGS is not typically inherited in a simple Mendelian manner and often occurs sporadically.
- Developmental disorders: Children with developmental disorders, such as cerebral palsy or autism spectrum disorder, may be at increased risk of developing LGS.
- Infections: Infections such as meningitis or encephalitis can lead to brain damage and increase the risk of developing epilepsy, including LGS.
- Metabolic disorders: Certain metabolic disorders, such as mitochondrial disease or phenylketonuria (PKU), may be associated with an increased risk of developing LGS.
- Hypoxic-ischemic injury: Lack of oxygen or blood flow to the brain, either during birth or due to other factors, can lead to brain damage and increase the risk of developing epilepsy, including LGS.
- Unknown factors: In many cases, the exact cause of LGS is unknown, and the condition appears to develop spontaneously without a clear underlying cause.
It’s important to note that while these factors may increase the risk of developing LGS, not all individuals with these risk factors will develop the condition. LGS is a complex and multifactorial disorder, and further research is needed to fully understand its causes and risk factors.
What is the treatment for Lennox-Gastaut syndrome?
The treatment for Lennox-Gastaut syndrome (LGS) typically involves a combination of medications, dietary therapy, and supportive care to manage seizures, improve quality of life, and address any associated developmental or behavioral issues. Treatment options for LGS may include:
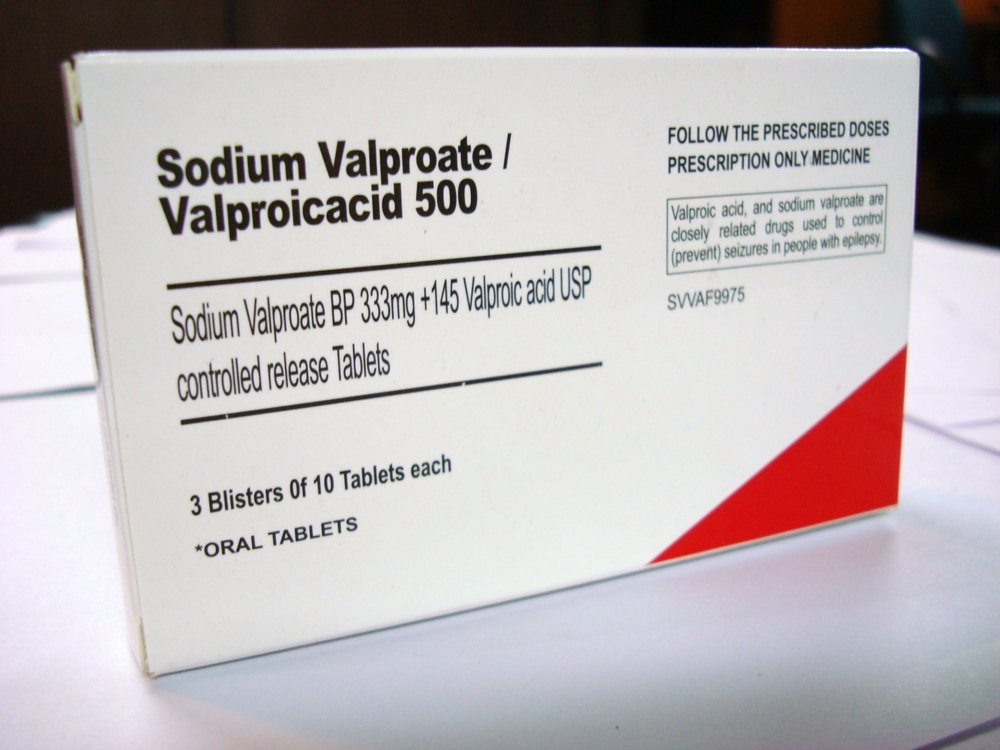
- Antiseizure medications: A variety of antiseizure medications may be used to help control seizures in individuals with LGS. These may include medications such as valproate, lamotrigine, topiramate, felbamate, and rufinamide. Polytherapy, or the use of multiple medications, is often necessary to adequately control seizures in LGS.
- Ketogenic diet: The ketogenic diet is a high-fat, low-carbohydrate diet that has been shown to be effective in reducing seizures in some individuals with LGS. It is typically used when medications are not effective or are poorly tolerated.
- Vagus nerve stimulation (VNS): Vagus nerve stimulation is a surgical procedure in which a device is implanted under the skin of the chest and connected to the vagus nerve in the neck. The device delivers electrical impulses to the brain to help reduce seizures.
- Responsive neurostimulation (RNS): RNS is a newer treatment option that involves the implantation of a device in the brain that can detect and respond to abnormal electrical activity, potentially reducing the frequency and severity of seizures.
- Corticosteroids: In some cases, corticosteroids such as prednisone may be used to help reduce inflammation and control seizures in individuals with LGS.
- Behavioral and developmental interventions: Individuals with LGS may benefit from behavioral and developmental interventions to help address cognitive and behavioral issues associated with the condition.
- Supportive care: Supportive care, such as physical therapy, occupational therapy, and speech therapy, can help improve quality of life and functional abilities in individuals with LGS.
- Management of comorbidities: Individuals with LGS may have comorbidities such as intellectual disability, behavioral problems, or sleep disturbances that require additional management.
Treatment for LGS is often complex and individualized, and it may require ongoing adjustments to achieve optimal seizure control and quality of life. It’s important for individuals with LGS to work closely with a healthcare team that is familiar with the condition to develop a comprehensive treatment plan.