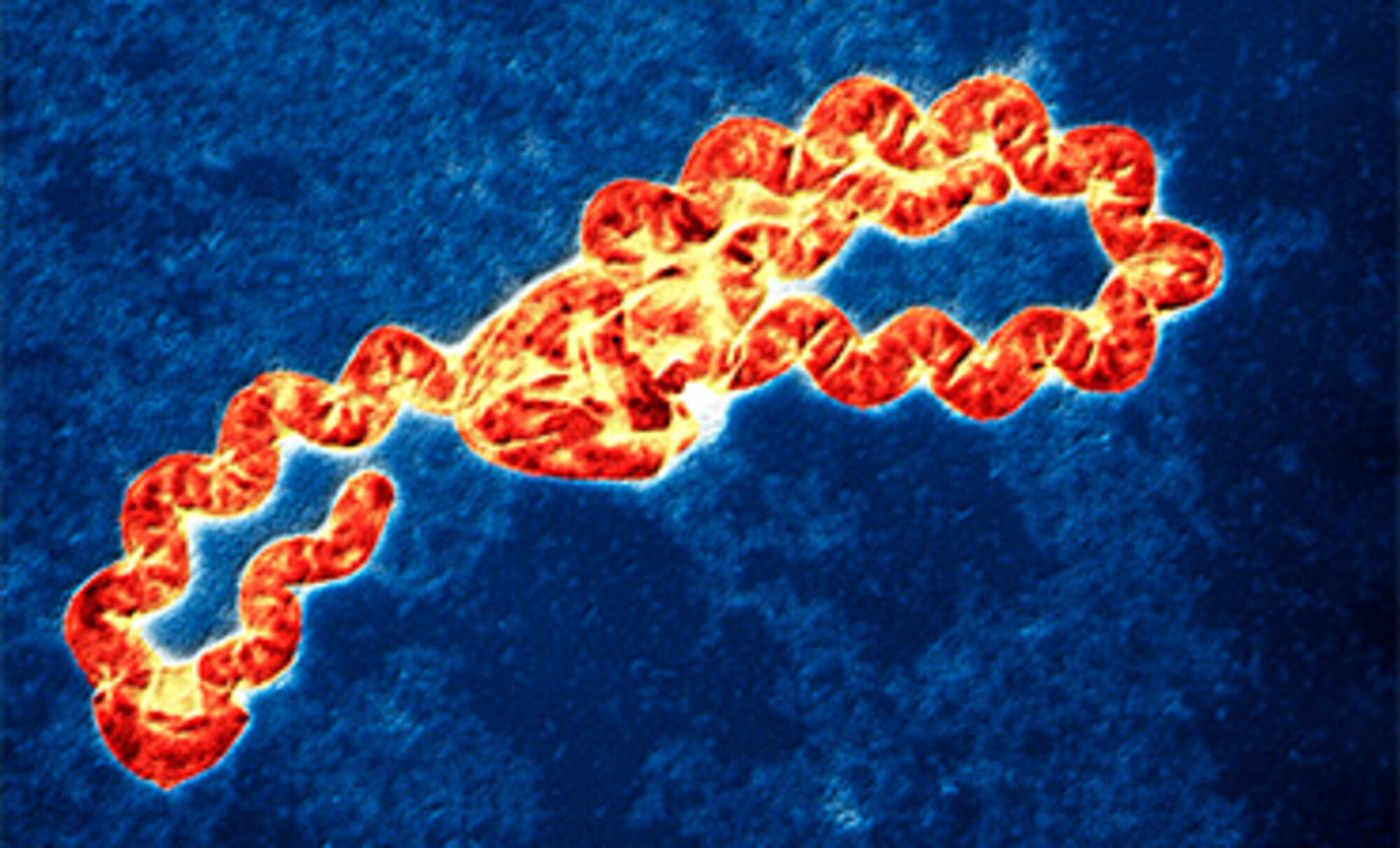
Leptospirosis: Symptoms, Causes & Treatment
What are the symptoms of leptospirosis?
Leptospirosis is a bacterial infection caused by bacteria of the genus Leptospira. The symptoms of leptospirosis can vary widely, and some infected individuals may not have any symptoms at all. When symptoms do occur, they can range from mild to severe and may include:
- High Fever: Sudden onset of high fever, often above 102°F (39°C).
- Muscle Aches: Severe muscle pain, particularly in the calves and lower back.
- Headache: Intense headache, often described as a pounding or throbbing sensation.
- Chills: Chills and shivering.
- Jaundice: Yellowing of the skin and eyes (jaundice) due to liver involvement.
- Red Eyes: Redness in the eyes (conjunctival suffusion).
- Abdominal Pain: Abdominal pain, nausea, vomiting, and diarrhea.
- Rash: Some people may develop a rash, which can vary in appearance from pinpoint red spots to a more widespread rash.
- Cough: Cough, chest pain, and difficulty breathing (in severe cases).
- Meningitis: In some cases, leptospirosis can lead to meningitis, which can cause symptoms such as severe headache, stiff neck, and sensitivity to light.
Symptoms of leptospirosis usually appear 5 to 14 days after exposure to the bacteria, but they can appear as early as 2 days or as late as 30 days after exposure. In some cases, leptospirosis can lead to severe complications, such as kidney damage, liver failure, respiratory distress, and even death. If you suspect you have leptospirosis, it’s important to seek medical attention promptly for diagnosis and treatment.
What are the causes of leptospirosis?
Leptospirosis is caused by bacteria of the genus Leptospira. These bacteria are typically found in the urine of infected animals, including rodents, cattle, pigs, dogs, and wild animals. The bacteria can survive in water and soil for weeks to months, and humans can become infected through contact with contaminated water, soil, or food, or through contact with the urine of infected animals.
Common ways people can become infected include:
- Direct Contact: Direct contact with the urine of infected animals, especially through cuts or abrasions on the skin or mucous membranes.
- Contaminated Water: Swimming, wading, or kayaking in water contaminated with Leptospira bacteria.
- Contaminated Soil: Working in or handling soil contaminated with urine from infected animals.
- Consumption of Contaminated Food or Water: Eating or drinking food or water contaminated with Leptospira bacteria.
- Animal Bites: Bites from infected animals, although this is less common.
Leptospirosis is more common in tropical and subtropical regions, especially in areas with high rainfall and flooding, which can lead to increased contamination of water and soil. Outdoor activities such as hiking, camping, and farming can also increase the risk of exposure to Leptospira bacteria.
What is the treatment for leptospirosis?
The treatment for leptospirosis usually involves antibiotics and supportive care. The choice of antibiotic and duration of treatment may vary depending on the severity of the infection and other factors. Common treatments include:
- Antibiotics: The antibiotic of choice for treating leptospirosis is usually doxycycline or penicillin. Other antibiotics, such as azithromycin or ceftriaxone, may be used in cases of severe disease or if the patient is unable to take doxycycline or penicillin.
- Supportive Care: Supportive care may include rest, fluids, and medications to relieve symptoms such as fever, pain, and nausea.
- Hospitalization: Severe cases of leptospirosis may require hospitalization for monitoring and intravenous antibiotics.
- Complications Management: Complications of leptospirosis, such as kidney damage or respiratory distress, may require additional treatment.
Early treatment is important to prevent complications and reduce the severity of the infection. If you suspect you have leptospirosis, it’s important to seek medical attention promptly for diagnosis and treatment.