Metabolic Syndrome: Symptoms, Causes, Treatment
What are the symptoms of metabolic syndrome?
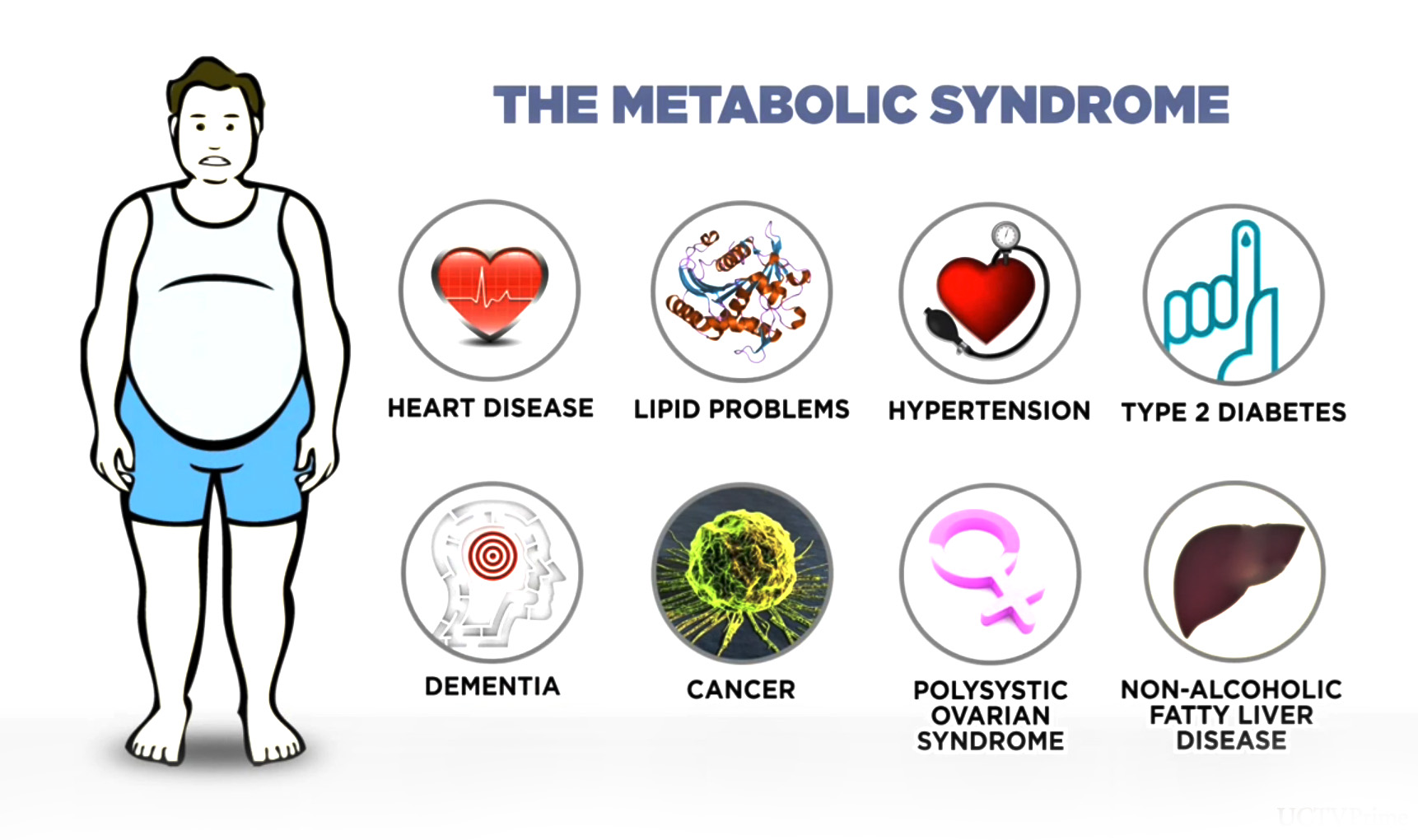
Metabolic syndrome is a cluster of conditions that occur together, increasing the risk of heart disease, stroke, and type 2 diabetes. The main symptoms and risk factors associated with metabolic syndrome include:
- Abdominal obesity: Excess fat in the abdominal area, often indicated by a waist circumference of 35 inches or more in women and 40 inches or more in men.
- High blood pressure: Blood pressure consistently higher than 130/85 mm Hg.
- High blood sugar: Fasting blood sugar level of 100 mg/dL or higher, indicating insulin resistance or prediabetes.
- High triglyceride levels: Triglyceride levels of 150 mg/dL or higher.
- Low HDL cholesterol levels: HDL (“good”) cholesterol levels below 50 mg/dL in women and below 40 mg/dL in men.
In addition to these symptoms and risk factors, people with metabolic syndrome may also experience other health issues, such as:
- Increased risk of cardiovascular disease: Metabolic syndrome significantly increases the risk of heart attack, stroke, and other cardiovascular diseases.
- Increased risk of type 2 diabetes: Insulin resistance, a key component of metabolic syndrome, can lead to type 2 diabetes if not managed.
- Increased risk of fatty liver disease: Metabolic syndrome is associated with an increased risk of non-alcoholic fatty liver disease (NAFLD).
- Increased risk of sleep apnea: People with metabolic syndrome are more likely to have sleep apnea, a condition characterized by interrupted breathing during sleep.
Metabolic syndrome is often related to lifestyle factors such as unhealthy diet, lack of physical activity, and excess weight. Making lifestyle changes, such as adopting a healthy diet, increasing physical activity, and losing weight, can help manage and prevent metabolic syndrome. Medications may also be prescribed to manage individual risk factors, such as high blood pressure or high cholesterol.
What are the causes of metabolic syndrome?
The exact causes of metabolic syndrome are not fully understood, but a combination of genetic and lifestyle factors are believed to play a role. Some of the key factors that contribute to the development of metabolic syndrome include:
- Insulin resistance: Insulin is a hormone that helps regulate blood sugar levels. In insulin resistance, cells in the body do not respond properly to insulin, leading to higher levels of insulin in the blood. This can contribute to the development of metabolic syndrome.
- Obesity: Excess body fat, particularly around the abdomen, is a major risk factor for metabolic syndrome. Fat tissue, especially around the abdomen, is metabolically active and can release substances that interfere with insulin action and promote inflammation.
- Physical inactivity: Lack of physical activity is strongly associated with metabolic syndrome. Regular physical activity helps improve insulin sensitivity and can help prevent or manage metabolic syndrome.
- Unhealthy diet: Diets high in refined carbohydrates, sugars, and unhealthy fats can contribute to the development of metabolic syndrome. These types of diets can lead to obesity, insulin resistance, and other metabolic abnormalities.
- Genetics: Some people may be genetically predisposed to develop metabolic syndrome. Family history of diabetes, obesity, or heart disease can increase the risk.
- Aging: The risk of metabolic syndrome increases with age, partly due to changes in hormone levels and a decrease in muscle mass and physical activity.
- Other medical conditions: Certain medical conditions, such as polycystic ovary syndrome (PCOS), sleep apnea, and fatty liver disease, are associated with an increased risk of metabolic syndrome.
- Ethnicity: Some ethnic groups, such as African Americans, Hispanics, and Native Americans, have a higher risk of developing metabolic syndrome.
While these factors can increase the risk of metabolic syndrome, making lifestyle changes such as adopting a healthy diet, increasing physical activity, and losing weight can help prevent or manage the condition. Medications may also be prescribed to help manage individual risk factors, such as high blood pressure or high cholesterol.
What is the treatment for metabolic syndrome?
The treatment for metabolic syndrome focuses on addressing the underlying risk factors to reduce the risk of heart disease, stroke, and type 2 diabetes. Treatment strategies may include:
- Lifestyle changes: Lifestyle modifications are the cornerstone of treatment for metabolic syndrome. These may include:
- Adopting a healthy diet rich in fruits, vegetables, whole grains, and lean proteins, and low in saturated fats, trans fats, cholesterol, and sodium.
- Engaging in regular physical activity, aiming for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening exercises on two or more days a week.
- Achieving and maintaining a healthy weight. Losing even a modest amount of weight can help improve insulin resistance, blood pressure, and cholesterol levels.
- Medications: In some cases, medications may be prescribed to help manage individual risk factors associated with metabolic syndrome, such as:
- Medications to lower blood pressure, such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, or diuretics.
- Medications to lower cholesterol levels, such as statins or fibrates.
- Medications to control blood sugar levels, such as metformin or insulin, if diabetes is present.
- Monitoring: Regular monitoring of blood pressure, cholesterol levels, and blood sugar levels is important for managing metabolic syndrome and assessing the effectiveness of treatment.
- Smoking cessation: If you smoke, quitting smoking is essential to reduce the risk of cardiovascular disease and other complications associated with metabolic syndrome.
- Management of other conditions: Managing other medical conditions, such as sleep apnea, fatty liver disease, or polycystic ovary syndrome (PCOS), which may contribute to metabolic syndrome, is also important.
- Regular follow-up: Regular follow-up with a healthcare provider is important to monitor progress, adjust treatment as needed, and address any new or worsening symptoms.
It’s important to work closely with a healthcare provider to develop a personalized treatment plan for metabolic syndrome based on individual risk factors and health needs. Making lifestyle changes and adhering to the treatment plan can help reduce the risk of complications and improve overall health and well-being.