MRSA Infection: Symptoms, Causes, Treatment
What are the symptoms of a methicillin-resistant Staphylococcus aureus (MRSA) infection?
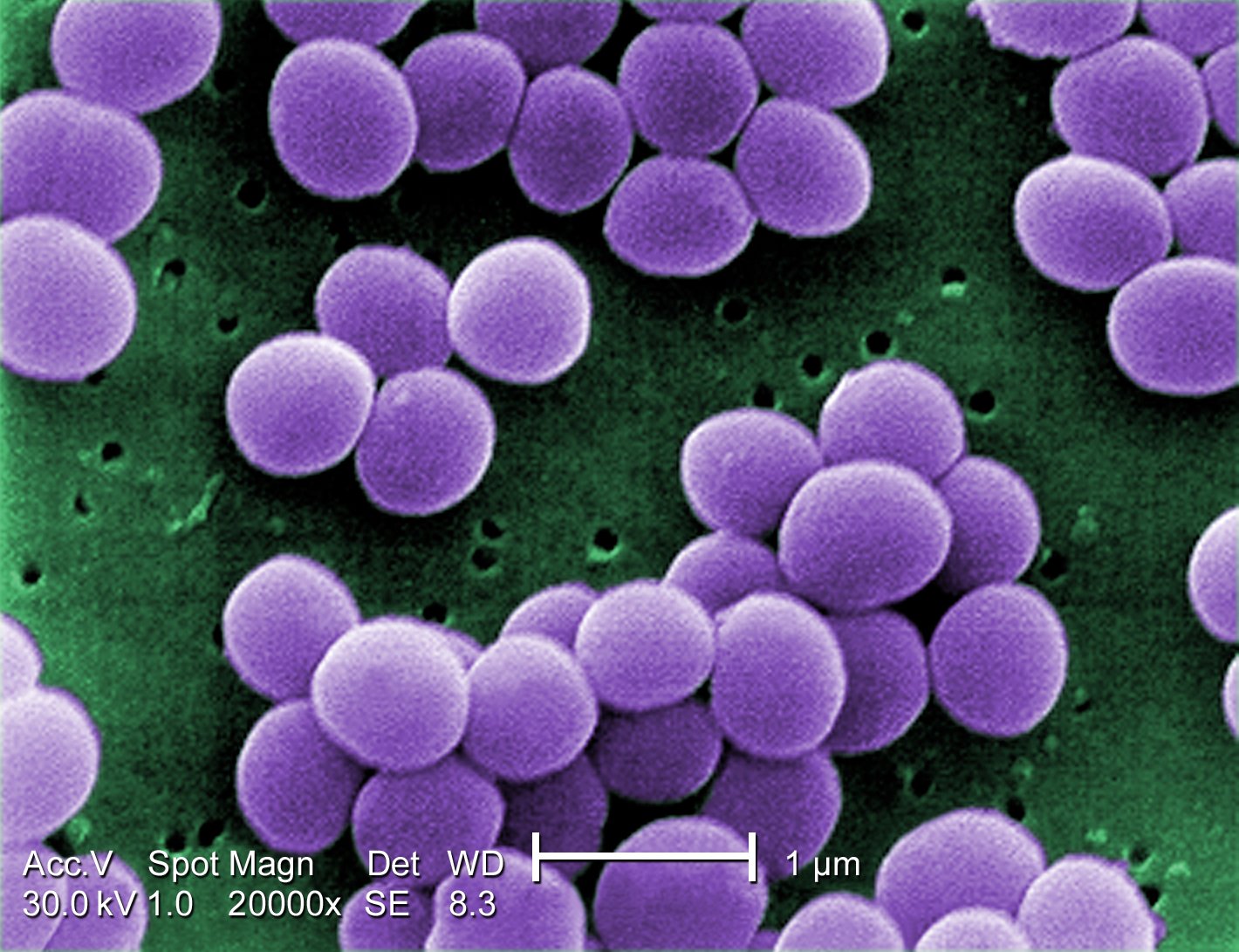
Methicillin-resistant Staphylococcus aureus (MRSA) is a type of staph bacteria that is resistant to certain antibiotics, including methicillin and other common antibiotics such as penicillin, amoxicillin, and oxacillin. MRSA can cause a range of symptoms, depending on the site and severity of the infection. Common symptoms of MRSA infections include:
- Skin Infections: MRSA commonly causes skin infections, such as boils, abscesses, cellulitis (inflammation of the skin and underlying tissue), and impetigo (a highly contagious skin infection).
- Wound Infections: MRSA can cause infections in surgical wounds, traumatic wounds, or other types of skin wounds. These infections can be more severe than those caused by other types of bacteria.
- Pneumonia: In some cases, MRSA can cause pneumonia, particularly in people who are hospitalized or have weakened immune systems.
- Bloodstream Infections (Bacteremia): MRSA can cause infections in the bloodstream, which can be life-threatening if not treated promptly.
- Bone Infections (Osteomyelitis): MRSA can infect bones, particularly in people with open fractures or other types of bone injuries.
- Joint Infections (Septic Arthritis): MRSA can infect joints, leading to pain, swelling, and decreased range of motion in the affected joint.
- Soft Tissue Infections: MRSA can cause infections in the soft tissues of the body, such as muscles and tendons.
Symptoms of MRSA infections can vary depending on the type and location of the infection. In general, symptoms of a MRSA infection may include:
- Redness, warmth, swelling, and tenderness at the site of the infection
- Pus or drainage from the site of the infection
- Fever
- Chills
- Fatigue
- Malaise (feeling generally unwell)
It’s important to seek medical attention if you suspect you have a MRSA infection, especially if you have a weakened immune system or are at higher risk of complications. MRSA infections can be serious and may require treatment with specific antibiotics that are effective against MRSA.
What are the causes of an MRSA infection?
MRSA infections are caused by a type of Staphylococcus aureus bacteria that has become resistant to certain antibiotics, including methicillin and other common antibiotics such as penicillin, amoxicillin, and oxacillin. The development of MRSA is primarily due to the overuse and misuse of antibiotics, which has led to the selection of resistant strains of bacteria. Here are some key factors that contribute to the development of MRSA infections:
- Antibiotic Use: Overuse and misuse of antibiotics can lead to the development of antibiotic-resistant bacteria, including MRSA. When antibiotics are used unnecessarily or are not taken as prescribed, bacteria can become resistant to the antibiotics, making them less effective.
- Healthcare Settings: MRSA is commonly associated with healthcare settings, such as hospitals, nursing homes, and long-term care facilities. People in these settings are at higher risk of developing MRSA infections due to frequent exposure to healthcare providers and medical procedures.
- Community Settings: Community-associated MRSA (CA-MRSA) has become more common in recent years and can affect healthy individuals who have not been hospitalized or had recent medical procedures. CA-MRSA is often spread through skin-to-skin contact or contact with contaminated surfaces.
- Close Contact: MRSA can spread through close contact with an infected person or by sharing personal items, such as towels, razors, or athletic equipment, that have come into contact with infected skin.
- Compromised Immune System: People with weakened immune systems, such as those with HIV/AIDS, cancer, or chronic illnesses, are at higher risk of developing MRSA infections.
- Crowded or Unsanitary Conditions: Living or working in crowded or unsanitary conditions can increase the risk of MRSA transmission.
- Invasive Medical Procedures: Certain invasive medical procedures, such as surgery, dialysis, or the use of indwelling catheters, can increase the risk of MRSA infections.
Preventing MRSA infections involves practicing good hygiene, avoiding unnecessary antibiotic use, and taking precautions to reduce the spread of bacteria in healthcare and community settings.
What is the treatment for an MRSA infection?
The treatment for an MRSA (Methicillin-resistant Staphylococcus aureus) infection depends on the severity of the infection and the site of the infection. MRSA infections can range from mild skin infections to more severe, life-threatening infections. Here are some common treatment options for MRSA infections:
- Skin and Soft Tissue Infections: For mild skin infections, such as boils or abscesses, drainage of the infected area may be sufficient. In addition, topical antibiotics or oral antibiotics other than beta-lactams (e.g., clindamycin, trimethoprim-sulfamethoxazole) may be prescribed. For more severe skin infections, intravenous (IV) antibiotics may be necessary.
- Invasive Infections (e.g., Pneumonia, Bloodstream Infections): Invasive MRSA infections, such as pneumonia or bloodstream infections, are typically treated with IV antibiotics, such as vancomycin, daptomycin, linezolid, or ceftaroline. The choice of antibiotic depends on the specific circumstances of the infection and the results of susceptibility testing.
- Surgical Drainage: In cases where an MRSA infection has formed an abscess or a collection of pus, surgical drainage may be necessary to remove the infected material and promote healing.
- Wound Care: Proper wound care, including cleaning and dressing of the infected area, is important to prevent further infection and promote healing.
- Supportive Care: In severe cases of MRSA infection, supportive care in a hospital setting may be necessary. This can include intravenous fluids, oxygen therapy, and other supportive measures.
It’s important to note that MRSA infections can be difficult to treat, as the bacteria are resistant to many antibiotics. Treatment may require a combination of antibiotics or prolonged courses of antibiotics. In some cases, the infection may recur or become chronic.
Prevention of MRSA infections is also important, especially in healthcare settings. This includes practicing good hand hygiene, using contact precautions when caring for patients with MRSA, and avoiding unnecessary antibiotic use.