Necrotizing Fasciitis: Symptoms, Causes, Treatment
What are the symptoms of necrotizing fasciitis?
Necrotizing fasciitis, commonly known as flesh-eating bacteria, is a serious bacterial infection that affects the skin, underlying tissue, and fascia (connective tissue that surrounds muscles, nerves, and blood vessels). The symptoms of necrotizing fasciitis can develop rapidly and may include:
- Severe pain: The affected area may be extremely painful, often out of proportion to the visible signs of infection.
- Swelling: Swelling and redness may occur rapidly in the affected area.
- Fever: A fever, sometimes accompanied by chills and sweating, may develop as the infection progresses.
- Skin changes: The skin over the affected area may become discolored, ranging from red to purple or blue, and may develop a shiny or glossy appearance.
- Ulcers, blisters, or black spots: The skin may develop ulcers, blisters filled with dark fluid, or black spots indicating tissue death (necrosis).
- Fatigue and weakness: As the infection spreads and the body’s immune response is activated, fatigue and weakness may occur.
- Nausea, vomiting, and diarrhea: Some individuals with necrotizing fasciitis may experience gastrointestinal symptoms as a result of the infection.
- Systemic symptoms: In severe cases, necrotizing fasciitis can lead to sepsis, a life-threatening condition characterized by an overwhelming immune response to infection. Symptoms of sepsis include rapid heart rate, rapid breathing, confusion, and a decrease in urine output.
It’s important to seek immediate medical attention if you experience symptoms of necrotizing fasciitis, especially if you have recently had a wound or injury that could have become infected. Necrotizing fasciitis is a medical emergency that requires prompt treatment with antibiotics and surgical intervention to remove the infected tissue.
What are the causes of necrotizing fasciitis?
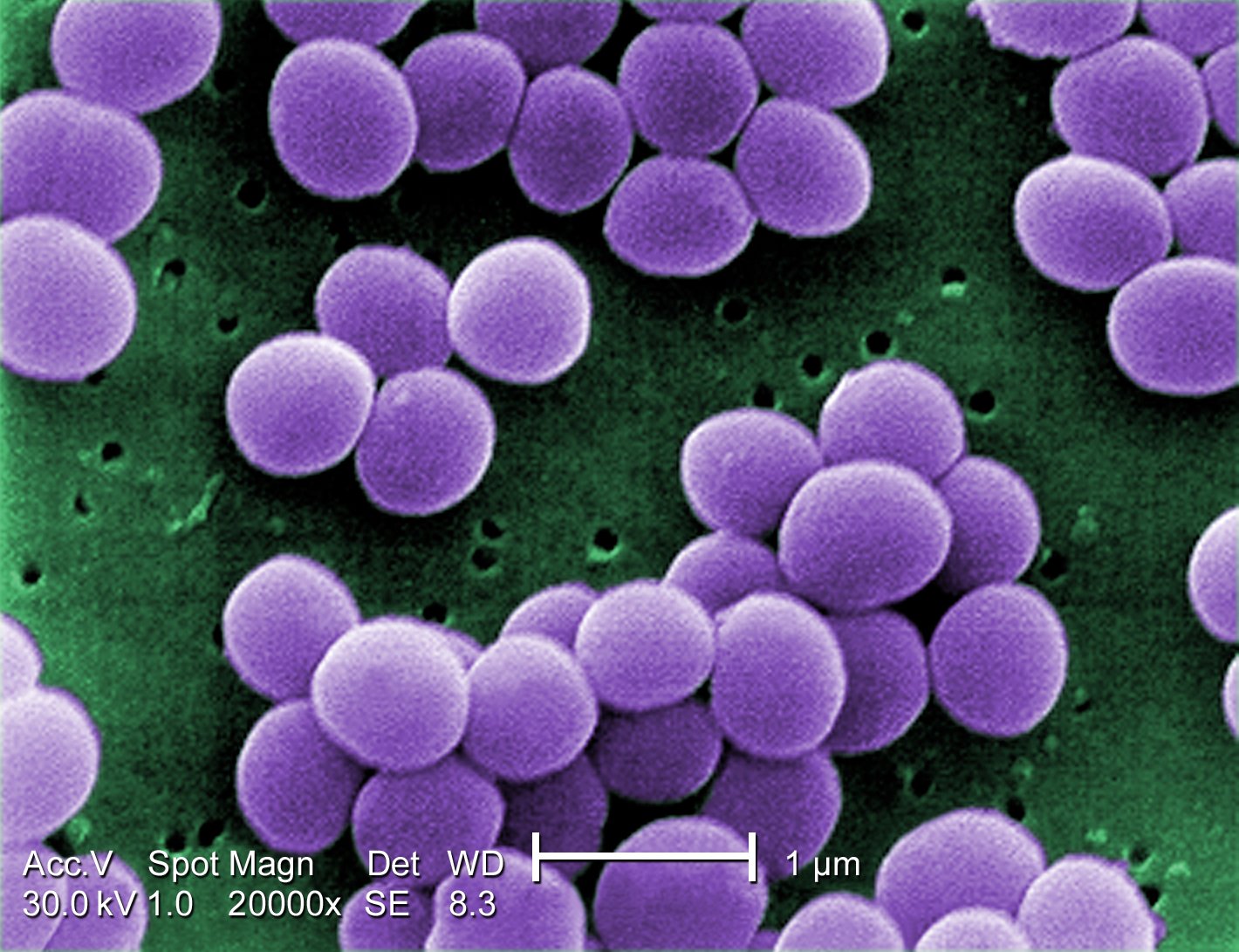
Necrotizing fasciitis is primarily caused by certain types of bacteria, most commonly group A Streptococcus (GAS) bacteria. Other bacteria, such as Staphylococcus aureus, Vibrio vulnificus, Clostridium perfringens, and others, can also cause necrotizing fasciitis, either alone or in combination with other bacteria.
These bacteria can enter the body through breaks in the skin, such as cuts, scrapes, burns, insect bites, surgical wounds, or puncture wounds. Once inside the body, the bacteria multiply and release toxins that damage the surrounding tissue and fascia (connective tissue surrounding muscles, nerves, and blood vessels), leading to the characteristic symptoms of necrotizing fasciitis.
Several factors can increase the risk of developing necrotizing fasciitis, including:
- Weakened immune system: Conditions or treatments that weaken the immune system, such as diabetes, cancer, chemotherapy, or long-term steroid use, can increase the risk of infection.
- Chronic health conditions: Chronic health conditions such as diabetes, peripheral vascular disease, or kidney disease can impair blood flow and increase the risk of infection.
- Alcoholism: Excessive alcohol consumption can weaken the immune system and increase the risk of infection.
- Obesity: Obesity can impair blood flow and increase the risk of infection.
- Malnutrition: Poor nutrition can weaken the immune system and increase the risk of infection.
- Recent surgery or injury: Recent surgical procedures or traumatic injuries can provide an entry point for bacteria to enter the body.
- IV drug use: Intravenous drug use can introduce bacteria into the body and increase the risk of infection.
It’s important to note that while certain factors can increase the risk of developing necrotizing fasciitis, the condition can occur in otherwise healthy individuals. Prompt medical attention by a specialist healthcare provider is crucial if necrotizing fasciitis is suspected, as the condition can progress rapidly and lead to serious complications.
What is the treatment for necrotizing fasciitis?
The treatment for necrotizing fasciitis, also known as flesh-eating bacteria infection, is aggressive and typically involves a combination of surgical intervention and antibiotic therapy. Prompt treatment is essential to prevent the infection from spreading and causing serious complications. Treatment may include:
- Surgical debridement: The primary treatment for necrotizing fasciitis is surgical removal (debridement) of the infected and dead tissue. This is done to stop the spread of the infection and to prevent further tissue damage. Multiple surgeries may be required to remove all infected tissue.
- Antibiotic therapy: Broad-spectrum antibiotics are administered intravenously to help fight the infection. The choice of antibiotics may be adjusted based on the results of cultures taken from the infected tissue.
- Supportive care: Patients with necrotizing fasciitis often require intensive care support, including intravenous fluids, pain management, and monitoring of vital signs.
- Hyperbaric oxygen therapy: In some cases, hyperbaric oxygen therapy may be used to help improve oxygen delivery to the affected tissue and promote healing.
- Amputation: In severe cases where the infection has caused extensive tissue damage, amputation of the affected limb or body part may be necessary to prevent the spread of the infection.
- Wound care: After surgical debridement, careful wound care is essential to prevent further infection and promote healing. This may include regular cleaning and dressing changes.
- Intravenous immunoglobulin (IVIG): In some cases, IVIG may be used as an adjunctive treatment to help modulate the immune response and reduce inflammation.
The exact course of treatment for necrotizing fasciitis depends on the severity of the infection, the extent of tissue damage, and the overall health of the patient. Early diagnosis and prompt initiation of treatment are critical for improving outcomes and reducing the risk of complications.