Noninfectious Uveitis: Symptoms, Causes, Treatment
What are the symptoms of noninfectious uveitis?
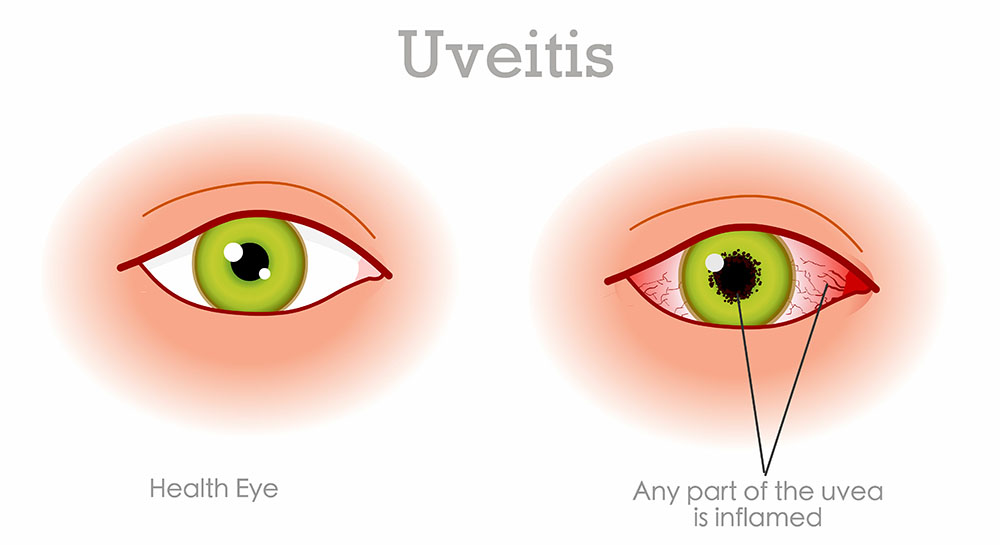
Noninfectious uveitis is inflammation of the uvea, the middle layer of the eye that includes the iris, ciliary body, and choroid. Symptoms of noninfectious uveitis can vary depending on the specific part of the uvea that is affected and the severity of the inflammation. Common symptoms may include:
- Eye Redness: Redness in one or both eyes, which may be mild or severe.
- Eye Pain: Pain in the affected eye or eyes, which may range from mild discomfort to severe, sharp pain.
- Blurry Vision: Blurred vision, which may be temporary or persistent.
- Sensitivity to Light: Increased sensitivity to light (photophobia), which may cause discomfort in bright light.
- Floaters: Floaters are small, dark spots or specks that appear to float in the field of vision.
- Loss of Vision: In severe cases, uveitis can lead to a loss of vision, especially if left untreated.
- Headaches: Some people with uveitis may experience headaches, especially if the inflammation is affecting the front of the eye.
- Eye Discharge: Discharge from the eye, which may be clear or slightly cloudy.
- Changes in Eye Color: In some cases, uveitis can cause the iris to change color, become mottled, or develop adhesions that affect the shape of the pupil.
It’s important to note that these symptoms can also be caused by other eye conditions, so it’s important to see an eye care professional for a proper diagnosis and treatment if you experience any of these symptoms. Untreated uveitis can lead to complications and permanent vision loss, so early detection and treatment are important.
What are the causes of noninfectious uveitis?
Noninfectious uveitis, also known as autoimmune uveitis, occurs when the body’s immune system attacks the tissues of the eye, leading to inflammation. The exact cause of noninfectious uveitis is not always clear, but it is thought to be related to an abnormal immune response. Some factors that may contribute to the development of noninfectious uveitis include:
- Autoimmune Diseases: Noninfectious uveitis is often associated with autoimmune diseases, such as rheumatoid arthritis, lupus, ankylosing spondylitis, and inflammatory bowel disease. In these conditions, the immune system mistakenly attacks healthy tissues, including those in the eye.
- Genetic Factors: Some people may have a genetic predisposition to developing uveitis, although the specific genes involved are not yet fully understood.
- Environmental Factors: Exposure to certain environmental factors, such as toxins or allergens, may trigger an abnormal immune response leading to uveitis in susceptible individuals.
- Inflammatory Response to Infection: In some cases, uveitis may occur as a result of an inflammatory response to an infection, even though the infection itself may not be present in the eye.
- Other Systemic Conditions: Uveitis can also be associated with other systemic conditions, such as sarcoidosis, Behçet’s disease, and Vogt-Koyanagi-Harada (VKH) syndrome.
- Eye Trauma or Surgery: Uveitis can sometimes occur as a result of eye trauma or surgery, although this is less common.
It’s important to note that while infections can cause uveitis, noninfectious uveitis is not caused by an infection. Instead, it is a result of an abnormal immune response. The specific cause of uveitis can vary from person to person, and in many cases, the exact cause may not be identified. Treatment for noninfectious uveitis typically focuses on reducing inflammation and managing symptoms.
What is the treatment for noninfectious uveitis?
Treatment for noninfectious uveitis aims to reduce inflammation, relieve symptoms, prevent complications, and preserve vision. The specific treatment approach depends on the severity of the uveitis, the part of the eye affected, and the underlying cause. Treatment options may include:
- Corticosteroid Eye Drops: Corticosteroid eye drops are often used to reduce inflammation and relieve symptoms. They are usually the first line of treatment for mild to moderate uveitis.
- Oral Corticosteroids: In cases of more severe uveitis or when eye drops alone are not effective, oral corticosteroids may be prescribed to reduce inflammation throughout the body.
- Steroid Injections: Steroid injections around the eye or into the vitreous (the gel-like substance inside the eye) may be used for more targeted treatment of inflammation.
- Immunosuppressive Medications: If corticosteroids alone are not effective or if long-term treatment is needed, immunosuppressive medications such as methotrexate, azathioprine, or mycophenolate mofetil may be used to suppress the immune response and reduce inflammation.
- Biologic Agents: In some cases, biologic agents such as adalimumab or infliximab may be used to target specific proteins involved in the inflammatory process.
- Surgery: In certain situations, surgery may be necessary to remove scar tissue or repair damage caused by uveitis. Surgery may also be needed to treat complications such as glaucoma or cataracts that can occur as a result of uveitis.
- Lifestyle Changes: Making lifestyle changes such as quitting smoking, maintaining a healthy weight, and managing underlying conditions such as diabetes or high blood pressure can help improve overall health and may reduce the risk of uveitis flare-ups.
It’s important for individuals with uveitis to work closely with their healthcare providers to develop a treatment plan that is tailored to their specific needs. Regular eye exams and monitoring are essential to detect and manage uveitis flare-ups and prevent complications that could lead to vision loss.