Plantar Fasciitis: Symptoms, Causes, Treatment
What are the symptoms of plantar fasciitis?
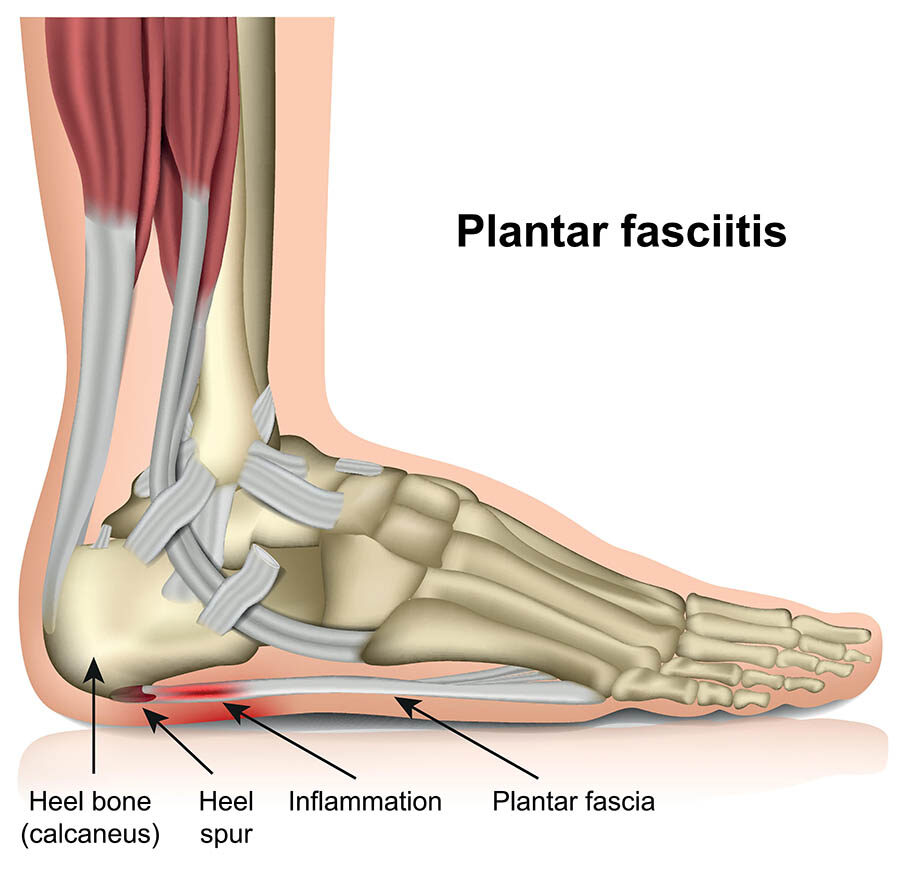
Plantar fasciitis is a common cause of heel pain that involves inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of your foot and connects your heel bone to your toes. The most common symptoms of plantar fasciitis include:
- Pain: The most prominent symptom of plantar fasciitis is pain on the bottom of the heel, which can be sharp, stabbing, or burning in nature. The pain is usually worst with the first few steps in the morning or after long periods of standing or sitting.
- Stiffness: Many people with plantar fasciitis experience stiffness and pain in the heel and foot, especially after periods of rest or inactivity.
- Tenderness: The bottom of the heel may be tender to the touch, and there may be swelling or redness in the area.
- Pain that worsens with activity: Plantar fasciitis pain typically worsens with activity, especially activities that involve prolonged standing, walking, or running.
- Pain that improves with rest: Resting the foot can help alleviate plantar fasciitis pain, but the pain may return when you resume activity.
- Pain that affects one foot: Plantar fasciitis usually affects only one foot, although it can occur in both feet simultaneously.
- Pain that develops gradually: The symptoms of plantar fasciitis often develop gradually over time, rather than suddenly.
It’s important to note that the symptoms of plantar fasciitis can vary from person to person, and not everyone with plantar fasciitis will experience all of these symptoms. If you are experiencing heel pain, especially if it is severe or persistent, it’s important to see a healthcare provider for an accurate diagnosis and appropriate treatment.
What are the causes of plantar fasciitis?
Plantar fasciitis is caused by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of your foot and connects your heel bone to your toes. The exact cause of plantar fasciitis is not always clear, but several factors may contribute to its development, including:
- Overuse or repetitive stress: Plantar fasciitis often occurs in people who engage in activities that put a lot of stress on the feet, such as running, dancing, or standing for long periods.
- Poor foot mechanics: Flat feet, high arches, or abnormal walking patterns can alter the way weight is distributed on the feet, putting strain on the plantar fascia.
- Tight calf muscles: Tight calf muscles can increase the strain on the plantar fascia and contribute to the development of plantar fasciitis.
- Obesity: Excess body weight can increase the strain on the plantar fascia and contribute to its inflammation.
- Improper footwear: Wearing shoes with inadequate support or cushioning, or shoes that are worn out, can increase the risk of plantar fasciitis.
- Age: Plantar fasciitis is more common in middle-aged and older adults, possibly due to the natural aging process and decreased flexibility of the plantar fascia.
- Certain activities: Participating in activities that involve repetitive pounding on the feet, such as running or aerobics, can increase the risk of plantar fasciitis.
- Foot structure: Certain foot conditions, such as high arches or flat feet, can increase the risk of plantar fasciitis.
- Occupational factors: Jobs that require prolonged standing or walking on hard surfaces can increase the risk of plantar fasciitis.
It’s important to address the underlying causes of plantar fasciitis to prevent it from recurring. This may include wearing supportive footwear, stretching exercises, orthotic devices, and modifying activities that aggravate the condition. In some cases, physical therapy or corticosteroid injections may be recommended to help reduce inflammation and pain.
What is the treatment for plantar fasciitis?
Treatment for plantar fasciitis typically focuses on relieving symptoms and reducing inflammation. Some common treatments and strategies that may be recommended include:
- Rest: Resting the affected foot and avoiding activities that worsen the pain can help reduce inflammation and promote healing.
- Ice: Applying ice to the affected area for 15-20 minutes several times a day can help reduce pain and inflammation.
- Stretching exercises: Stretching exercises for the calf muscles and plantar fascia can help improve flexibility and reduce strain on the plantar fascia.
- Footwear: Wearing supportive shoes with cushioned soles and good arch support can help reduce strain on the plantar fascia.
- Orthotic devices: Using orthotic devices, such as shoe inserts or heel pads, can help support the arch and reduce strain on the plantar fascia.
- Night splints: Wearing a night splint that stretches the calf and plantar fascia while you sleep can help reduce morning pain and stiffness.
- Physical therapy: Physical therapy may be recommended to help strengthen the muscles of the foot and leg and improve flexibility.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen may be recommended to help reduce pain and inflammation.
- Corticosteroid injections: In some cases, corticosteroid injections may be recommended to help reduce inflammation and pain.
- Extracorporeal shock wave therapy (ESWT): ESWT is a noninvasive procedure that uses shock waves to stimulate healing of the plantar fascia.
- Surgery: In severe cases of plantar fasciitis that do not respond to other treatments, surgery may be recommended to release the plantar fascia or remove bone spurs.
It’s important to work with a healthcare provider to develop a treatment plan that is tailored to your individual needs and circumstances. With proper treatment and care, most people with plantar fasciitis experience significant improvement in their symptoms.