Polymyalgia Rheumatica: Symptoms, Causes, Treatment
What are the symptoms of polymyalgia rheumatica?
Polymyalgia rheumatica (PMR) is an inflammatory disorder that causes muscle pain and stiffness, primarily in the shoulders and hips. The symptoms of PMR can vary from person to person but often include:
- Muscle pain: Persistent or worsening pain in the shoulders, upper arms, neck, hips, thighs, or lower back. The pain is typically worse in the morning or after periods of inactivity.
- Stiffness: Stiffness in the affected muscles, especially in the morning or after sitting or lying down for long periods. The stiffness can make it difficult to move or perform daily activities.
- Fatigue: Feeling tired or lacking energy, which can be a result of the underlying inflammation.
- Limited range of motion: Difficulty moving the affected joints, especially the shoulders and hips, due to pain and stiffness.
- Fever: Some people with PMR may experience a low-grade fever, especially at the onset of the condition.
- Weight loss: Unintentional weight loss may occur, particularly in severe cases.
- Depression or mood changes: Some people with PMR may experience depression or changes in mood, possibly due to the chronic pain and fatigue.
- Other symptoms: Some people with PMR may experience symptoms such as headaches, jaw pain (temporomandibular joint pain), or swelling in the hands and feet.
It’s important to note that the symptoms of PMR can develop suddenly or gradually and may vary in severity. PMR primarily affects people over the age of 50, and the symptoms can overlap with those of other conditions, so it’s important to see a healthcare provider for a proper diagnosis if you experience symptoms of PMR.
What are the causes of polymyalgia rheumatica?
The exact cause of polymyalgia rheumatica (PMR) is unknown, but it is believed to be an autoimmune disorder, which means that the body’s immune system mistakenly attacks its own tissues. Genetic, environmental, and hormonal factors may all play a role in the development of PMR. Some potential causes or triggers of PMR include:
- Genetics: There may be a genetic predisposition to developing PMR, as the condition tends to run in families.
- Immune system dysfunction: In people with PMR, the immune system may become overactive and attack the body’s own tissues, leading to inflammation in the muscles and other tissues.
- Environmental factors: Exposure to certain environmental factors, such as infections or toxins, may trigger an abnormal immune response in susceptible individuals.
- Hormonal factors: Hormonal changes, particularly a decrease in estrogen levels, may play a role in the development of PMR, as the condition is more common in women and often occurs after menopause.
- Other factors: Some researchers believe that factors such as stress, trauma, or injury may also contribute to the development of PMR, although more research is needed to fully understand these potential triggers.
It’s important to note that while these factors may increase the risk of developing PMR, they do not guarantee that a person will develop the condition. Many people with one or more risk factors do not develop PMR, and some people with no known risk factors do develop the condition.
What is the treatment for polymyalgia rheumatica?
The primary treatment for polymyalgia rheumatica (PMR) is medication to reduce inflammation and manage symptoms. The most commonly prescribed medications for PMR include:
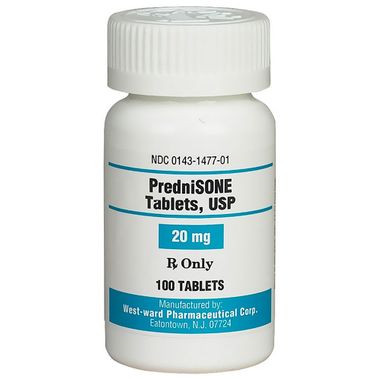
- Corticosteroids: Prednisone is the most commonly used corticosteroid for treating PMR. It helps reduce inflammation and relieve pain and stiffness. The dose is usually started at a higher level and gradually reduced as symptoms improve. Long-term use of corticosteroids can have side effects, so the lowest effective dose is used for the shortest possible time.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs such as ibuprofen or naproxen may be used to help reduce pain and inflammation in people with PMR. However, they are usually not as effective as corticosteroids for managing PMR symptoms.
- Disease-modifying antirheumatic drugs (DMARDs): In some cases, DMARDs such as methotrexate may be used in combination with corticosteroids to help reduce the dose of corticosteroids needed to control symptoms. This can help reduce the risk of long-term side effects from corticosteroid use.
- Biologic therapies: Biologic medications, such as tocilizumab, may be used in people with PMR who do not respond well to corticosteroids or other treatments. These medications target specific proteins in the immune system to help reduce inflammation.
- Physical therapy: Physical therapy can help improve flexibility, strength, and range of motion in people with PMR. It can also help reduce pain and stiffness and improve overall function.
- Lifestyle changes: Making lifestyle changes such as getting regular exercise, eating a healthy diet, and getting enough rest can help improve overall health and well-being in people with PMR.
It’s important for people with PMR to work closely with their healthcare providers to develop a treatment plan that is tailored to their individual needs. Regular monitoring and follow-up care are important to ensure that treatment is effective and to monitor for any potential side effects of medications.