Primary Biliary Cholangitis: Symptoms, Causes & Treatment
Primary Biliary Cholangitis Symptoms
Primary biliary cholangitis (PBC), formerly known as primary biliary cirrhosis, is a chronic autoimmune liver disease that primarily affects women. The symptoms of PBC can vary, and some individuals may not experience any symptoms in the early stages. However, as the disease progresses, the following symptoms may occur:
- Fatigue: Extreme tiredness and lack of energy are among the most common symptoms of PBC, often occurring even before other symptoms become apparent.
- Itchy skin (pruritus): Many individuals with PBC experience intense, generalized itching, especially on the arms, legs, and trunk. This itching can be severe and disruptive, affecting sleep and quality of life.
- Jaundice: As the disease progresses, the buildup of bilirubin in the body can cause yellowing of the skin and the whites of the eyes (jaundice).
- Dry eyes and dry mouth: PBC can lead to decreased tear and saliva production, resulting in dry eyes (keratoconjunctivitis sicca) and dry mouth (xerostomia).
- Abdominal pain: Some individuals with PBC may experience abdominal pain or discomfort, particularly in the upper right quadrant, due to inflammation or enlargement of the liver.
- Cholestasis: PBC can cause cholestasis, a condition characterized by the impaired flow of bile from the liver, leading to elevated levels of bile acids in the blood.
- Hyperlipidemia: Many individuals with PBC have elevated levels of cholesterol and triglycerides in the blood (hyperlipidemia).
- Xanthomas: These are yellowish deposits of cholesterol under the skin, often occurring on the eyelids or around the eyes.
- Osteoporosis: PBC can increase the risk of developing osteoporosis (a condition characterized by low bone density and an increased risk of fractures) due to the body’s impaired ability to absorb calcium and vitamin D.
- Hypothyroidism: Some individuals with PBC may also develop an underactive thyroid (hypothyroidism) due to the autoimmune nature of the disease.
It’s important to note that the symptoms of PBC can vary widely from person to person, and some individuals may remain asymptomatic for years. However, if left untreated, PBC can progress to liver cirrhosis, liver failure, and potentially life-threatening complications. Early diagnosis and treatment are crucial to manage the disease and prevent further liver damage.
Primary Biliary Cholangitis Causes
Primary biliary cholangitis (PBC) is an autoimmune liver disease, which means that it is caused by the body’s own immune system attacking and destroying the bile ducts in the liver. The exact cause of this autoimmune process is not fully understood, but several factors are believed to contribute to the development of PBC:
- Genetic predisposition: PBC tends to run in families, suggesting that genetic factors play a role in the development of the disease. Certain genetic variations, particularly in genes involved in immune regulation and bile acid metabolism, have been associated with an increased risk of PBC.
- Environmental triggers: While genetics may provide a predisposition, it is believed that environmental factors may trigger the autoimmune response in genetically susceptible individuals. Potential environmental triggers that have been proposed include:
- Infections (viral or bacterial)
- Exposure to chemicals or toxins
- Smoking
- Hormonal factors (PBC is more common in women, especially around menopause)
- Molecular mimicry: Some researchers believe that the immune system’s response to certain bacterial or viral proteins may cross-react with proteins found in the bile ducts, leading to an autoimmune attack on the bile ducts.
- Epigenetic factors: Epigenetic changes, which are modifications in gene expression that do not involve changes in the DNA sequence itself, may play a role in the development of PBC by altering the regulation of immune system genes.
- Gut microbiome: There is growing evidence that alterations in the gut microbiome (the collective community of microorganisms in the intestines) may contribute to the development of autoimmune diseases, including PBC, by influencing the immune system.
It is important to note that PBC is not caused by a single factor but rather by a complex interplay of genetic, environmental, and immunological factors. The exact mechanisms that trigger the autoimmune response and destruction of the bile ducts in PBC are not yet fully understood, and ongoing research is aimed at unraveling the underlying causes and pathways involved in this condition.
While the causes of PBC are not entirely clear, identifying risk factors and understanding the immunological processes involved can help in the development of more effective treatments and potential preventive strategies for this chronic liver disease.
Primary Biliary Cholangitis Treatment
The treatment for primary biliary cholangitis (PBC) aims to slow the progression of the disease, manage symptoms, and prevent complications. The main treatment approaches include:
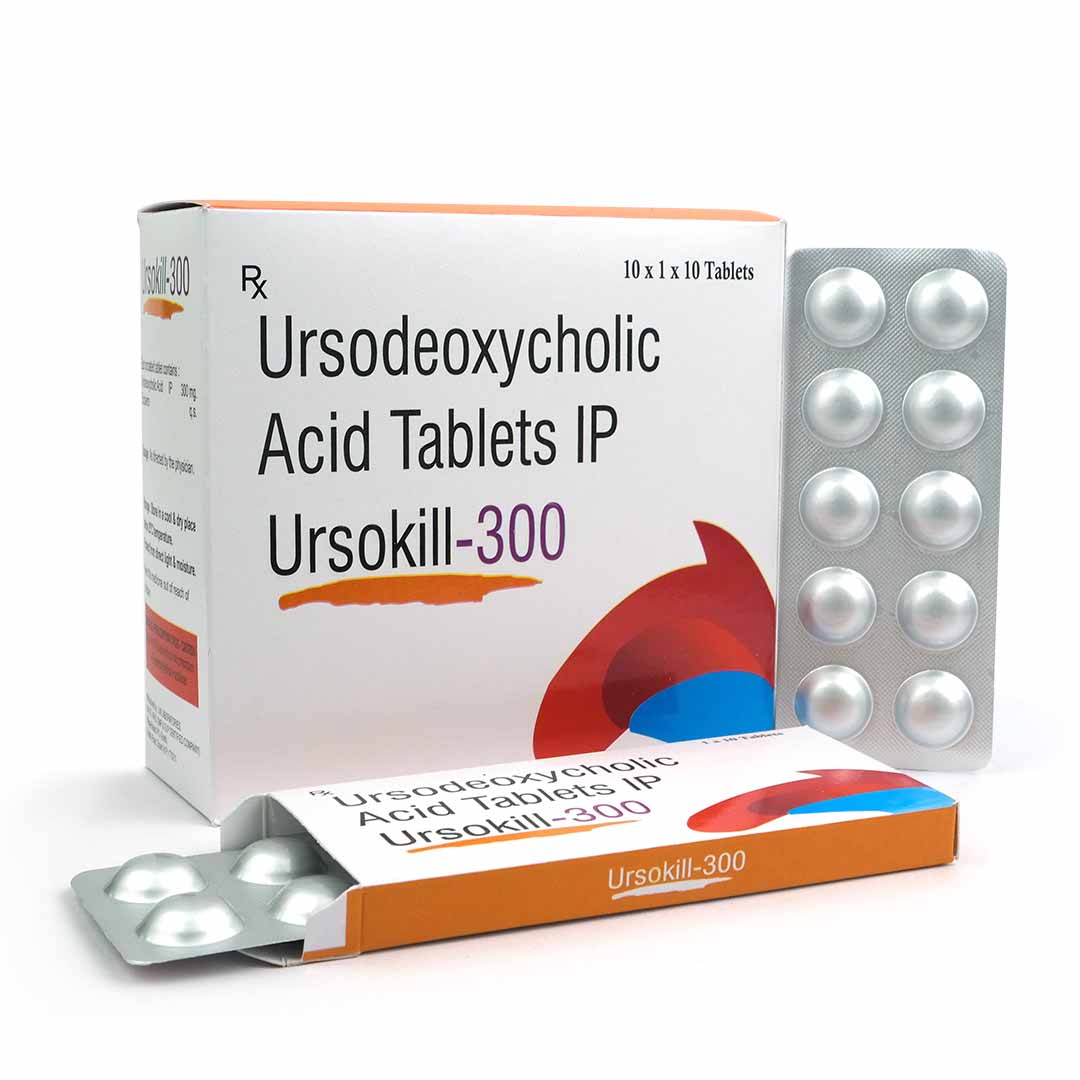
- Ursodeoxycholic acid (UDCA): This is the primary medication used to treat PBC. UDCA is a bile acid that helps to improve bile flow, reduce liver inflammation, and slow the progression of liver damage. It is typically prescribed at a dose of 13-15 mg per kilogram of body weight per day.
- Obeticholic acid (OCA): If UDCA alone is not effective in controlling the disease, OCA may be added as a second-line treatment. OCA is a semi-synthetic bile acid that can further improve bile flow and liver function in PBC patients.
- Immunosuppressants: In some cases, immunosuppressant drugs, such as methotrexate or budesonide, may be used to help suppress the autoimmune response and reduce liver inflammation. However, their use is generally limited due to potential side effects.
- Symptom management:
- Cholestyramine or colestipol: These bile acid sequestrants can help relieve severe itching (pruritus) associated with PBC.
- Antihistamines or gabapentin: These medications may also be used to manage itching.
- Vitamin supplements: Individuals with PBC may require vitamin supplements, particularly fat-soluble vitamins (vitamin A, vitamin D, vitamin E, vitamin K), due to impaired bile flow and nutrient absorption.
- Liver transplantation: For patients with advanced liver disease or liver failure due to PBC, a liver transplant may be necessary. Liver transplantation can significantly improve survival and quality of life in these cases.
- Lifestyle modifications:
- Avoiding potential triggers: Patients may be advised to avoid smoking, alcohol, and certain medications or chemicals that could further stress the liver.
- Maintaining a healthy weight and diet: A balanced diet and maintaining a healthy weight can help reduce the burden on the liver.
- Regular exercise: Moderate exercise can help improve overall health and may have beneficial effects on liver function.
- Management of complications: Treatment may also involve managing complications associated with PBC, such as osteoporosis, hyperlipidemia, or portal hypertension, with appropriate medications and interventions.
The treatment approach for PBC is often individualized based on the patient’s age, disease severity, response to treatment, and the presence of any complications or comorbidities. Regular monitoring of liver function tests and disease progression is essential to adjust the treatment plan as needed. With proper management, many individuals with PBC can maintain a good quality of life and slow the progression of the disease.