Primary Sclerosing Cholangitis: Symptoms, Causes, Treatment
What are the symptoms of primary sclerosing cholangitis?
Primary sclerosing cholangitis (PSC) is a rare, chronic liver disease characterized by inflammation and scarring (fibrosis) of the bile ducts inside and outside the liver. The symptoms of PSC can vary widely from person to person, and some individuals may not experience any symptoms. When symptoms do occur, they can include:
- Fatigue: Feeling tired or weak, which can be a result of decreased liver function and bile flow.
- Itching (pruritus): Itching, especially on the hands and feet, due to the accumulation of bile salts in the bloodstream.
- Jaundice: Yellowing of the skin and eyes, caused by the buildup of bilirubin in the bloodstream.
- Abdominal pain: Discomfort or pain in the upper right quadrant of the abdomen, where the liver is located.
- Enlarged liver or spleen: The liver or spleen may become enlarged due to inflammation and scarring.
- Weight loss: Unintentional weight loss, which can occur due to decreased appetite and malabsorption of nutrients.
- Fever: Some individuals with PSC may experience fever, especially if there is an infection or inflammation present.
- Cholangitis: Recurrent episodes of cholangitis, which is an infection of the bile ducts, can occur in some individuals with PSC.
- Osteoporosis: Decreased absorption of vitamin D and calcium due to liver dysfunction can lead to osteoporosis.
- Complications: PSC can lead to complications such as gallstones, liver cirrhosis, liver failure, and an increased risk of liver cancer.
It’s important to note that the progression of PSC can be slow, and many individuals with the condition may not experience symptoms for years. PSC is a chronic condition that requires ongoing monitoring and management by a healthcare provider experienced in treating liver diseases.
What are the causes of primary sclerosing cholangitis?
The exact cause of primary sclerosing cholangitis (PSC) is unknown, but it is believed to be an autoimmune condition, where the body’s immune system mistakenly attacks the bile ducts in the liver. Several factors may contribute to the development of PSC, including:
- Autoimmune response: PSC is thought to be an autoimmune disease, where the immune system attacks the body’s own tissues. In PSC, the immune system targets the bile ducts, leading to inflammation and scarring.
- Genetic factors: There is evidence to suggest that genetic factors may play a role in the development of PSC. Certain genetic variations have been associated with an increased risk of developing the condition.
- Environmental factors: Some environmental factors, such as infections or toxins, may trigger or exacerbate the autoimmune response in susceptible individuals.
- Inflammatory bowel disease (IBD): PSC is strongly associated with inflammatory bowel disease, particularly ulcerative colitis. Up to 70% of individuals with PSC also have ulcerative colitis, and the presence of IBD increases the risk of developing PSC.
- Other factors: PSC may also be associated with other autoimmune conditions, such as autoimmune hepatitis, thyroid disorders, and celiac disease.
It’s important to note that while these factors may contribute to the development of PSC, the exact cause of the condition is not fully understood. PSC is a complex disease, and more research is needed to determine the underlying mechanisms and risk factors involved.
What is the treatment for primary sclerosing cholangitis?
Primary sclerosing cholangitis (PSC) is a chronic condition for which there is no cure. Treatment focuses on managing symptoms, preventing complications, and slowing the progression of the disease. Treatment options for PSC may include:
- Medications:
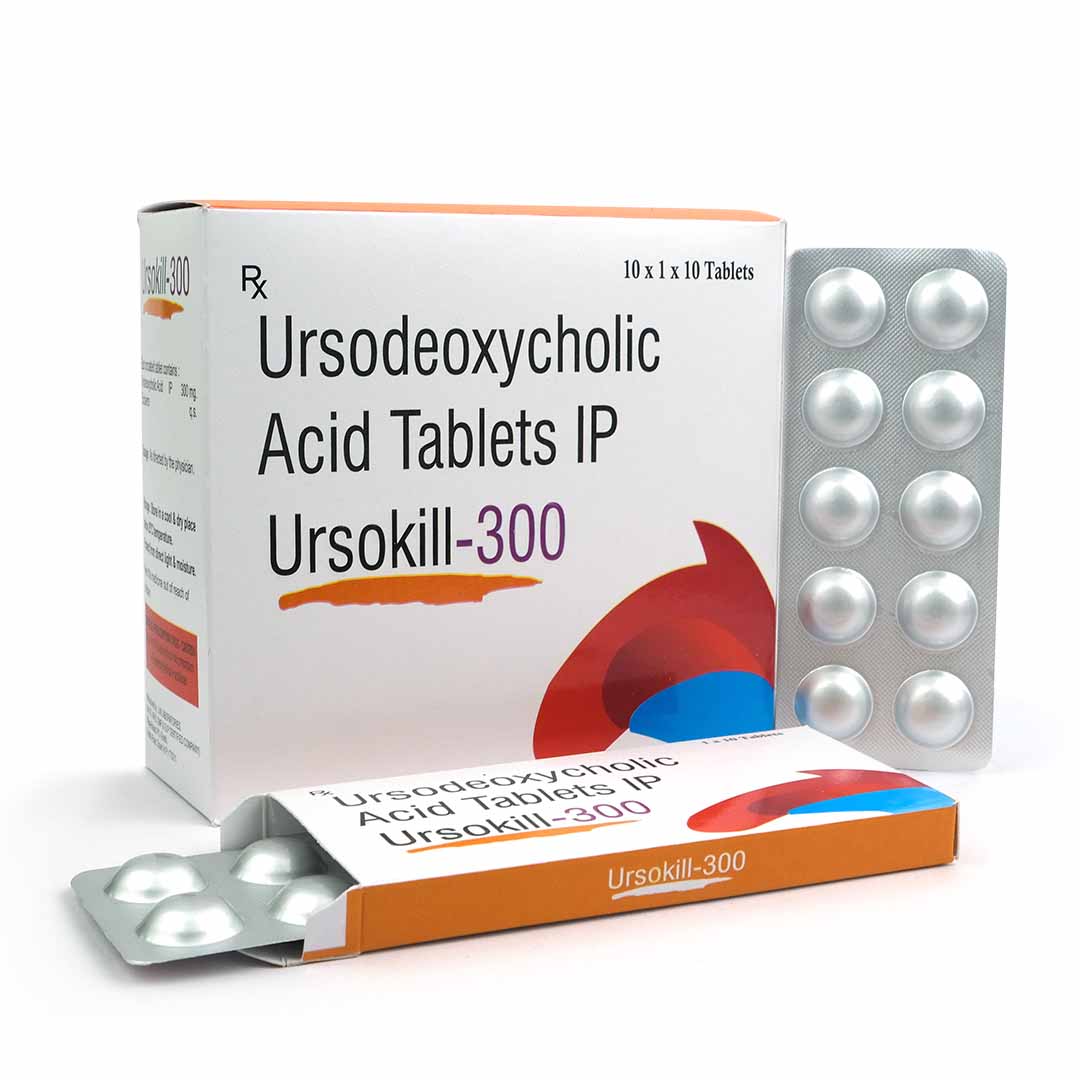
- Ursodeoxycholic acid (UDCA): This medication may help improve liver function and bile flow in some people with PSC, although it is not effective for everyone.
- Antibiotics: Antibiotics may be prescribed to treat bacterial infections that can occur in the bile ducts or liver.
- Anti-inflammatory medications: Medications such as corticosteroids or other anti-inflammatory drugs may be used to reduce inflammation in the bile ducts.
- Endoscopic therapy: Endoscopic retrograde cholangiopancreatography (ERCP) may be used to treat complications of PSC, such as bile duct strictures or stones, by opening or dilating the bile ducts.
- Liver transplant: In severe cases of PSC that progress to end-stage liver disease, a liver transplant may be necessary. A liver transplant can effectively cure PSC, but it is a major surgery with risks and lifelong implications.
- Management of complications: Treatment may be needed to manage complications of PSC, such as infections, bile duct strictures, or liver cirrhosis.
- Nutritional support: A healthy diet and nutritional supplements may be recommended to help manage symptoms and maintain overall health.
- Monitoring and surveillance: Regular monitoring and surveillance for complications of PSC, such as liver cancer, are important for managing the condition.
It’s important for individuals with PSC to work closely with a healthcare provider experienced in managing liver diseases to develop a personalized treatment plan. Treatment may need to be adjusted over time based on the individual’s symptoms, disease progression, and response to therapy. Early detection and treatment of complications are key to managing PSC effectively and improving quality of life.