Raynaud’s Disease: Symptoms, Causes, Treatment
What are the symptoms of Raynaud’s disease?
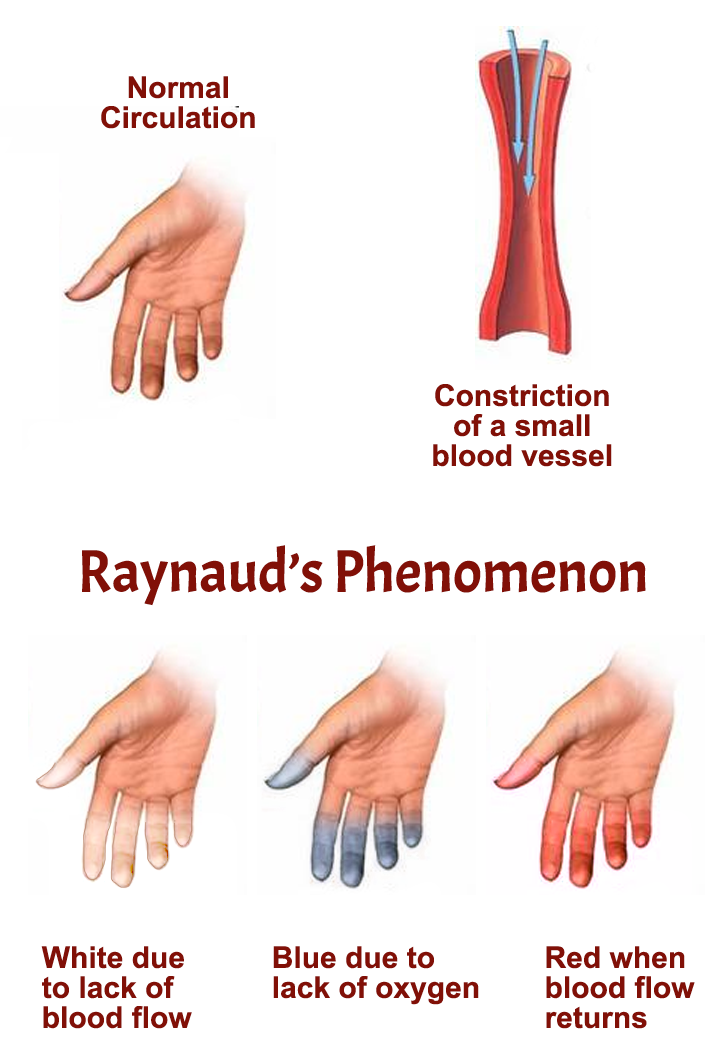
Raynaud’s disease, also known as Raynaud’s phenomenon or Raynaud’s syndrome, is a condition that affects blood flow to certain parts of the body, usually the fingers and toes, in response to cold temperatures or stress. It is characterized by episodic attacks called vasospasms, which cause the blood vessels in these areas to constrict, leading to reduced blood flow and color changes in the skin.
The main symptoms of Raynaud’s disease include:
- Color Changes: Affected areas may turn white or blue due to reduced blood flow, then red or purple as blood flow returns.
- Cold Sensitivity: The affected areas may feel cold and numb during an attack.
- Numbness or Tingling: Some people may experience numbness, tingling, or a pins-and-needles sensation in the affected areas.
- Pain or Throbbing: As blood flow returns, the affected areas may throb, tingle, or feel painful.
Raynaud’s disease can be primary, where the cause is unknown, or secondary, where it is associated with an underlying condition, such as autoimmune diseases (like lupus or scleroderma), injuries, medications, or exposure to certain chemicals.
While Raynaud’s disease itself is not usually serious, severe cases can lead to complications such as skin sores or ulcers, tissue death (gangrene), and, in rare cases, artery damage.
Management of Raynaud’s disease focuses on avoiding triggers and keeping affected areas warm. In some cases, medications to improve blood flow or reduce vasospasms may be prescribed. If you think you have Raynaud’s disease, you will need to consult your physician or specialist to obtain an accurate diagnosis.
What are the causes of Raynaud’s disease?
The exact cause of Raynaud’s disease is not fully understood, but it is believed to involve an exaggerated response of the blood vessels to cold or stress. During an attack of Raynaud’s, the blood vessels in the fingers and toes constrict more than normal in response to cold temperatures or emotional stress. This narrowing of the blood vessels reduces blood flow to the affected areas, leading to the characteristic color changes and symptoms of Raynaud’s disease.
There are two main types of Raynaud’s disease:
- Primary Raynaud’s: This is the most common form and occurs on its own, without an underlying medical condition. It is thought to be caused by an abnormal response of the blood vessels to cold or stress, but the exact trigger is not known.
- Secondary Raynaud’s: Also known as Raynaud’s phenomenon, this type is associated with an underlying medical condition or certain factors that can affect the blood vessels. These include autoimmune diseases (such as lupus or scleroderma), conditions that damage the arteries or nerves, certain medications, smoking, and exposure to certain chemicals.
In both types of Raynaud’s, the underlying mechanism involves an abnormal response of the blood vessels to cold or stress, leading to vasospasms and reduced blood flow to the affected areas. However, the specific triggers and mechanisms may vary between individuals.
What is the treatment for Raynaud’s disease?
Treatment for Raynaud’s disease focuses on reducing the frequency and severity of attacks, preventing complications, and improving blood flow to the affected areas. The approach to treatment may vary depending on the severity of the condition and whether it is primary or secondary Raynaud’s. Some common treatment options include:
- Lifestyle Changes: Avoiding cold temperatures and taking measures to keep the hands and feet warm, such as wearing gloves and warm socks, can help reduce the frequency of attacks. Managing stress and avoiding triggers, such as smoking and caffeine, may also be beneficial.
- Medications: In some cases, medications may be prescribed to help improve blood flow or reduce the frequency and severity of attacks. These may include calcium channel blockers, which relax and widen the blood vessels, or vasodilators, which help dilate the blood vessels. Other medications, such as alpha-blockers or PDE-5 inhibitors, may also be used in some cases.
- Biofeedback: Biofeedback techniques, which involve learning to control certain body responses, such as skin temperature and blood flow, may help some people with Raynaud’s disease.
- Surgery: In severe cases of Raynaud’s disease that do not respond to other treatments, surgery may be considered. This may involve cutting the nerves that control the blood vessels in the affected area (sympathectomy) or other procedures to improve blood flow.
- Other Therapies: Other therapies, such as nerve blocks, botox injections, or angioplasty, may be considered in some cases.
It’s important for individuals with Raynaud’s disease to work closely with their healthcare providers to develop a treatment plan that is tailored to their specific needs and to monitor for any complications. Regular follow-up visits may be necessary to adjust treatment as needed.