Spermatocele (Epididymal Cyst): Symptoms, Causes, Treatment
What are the symptoms of a spermatocele?
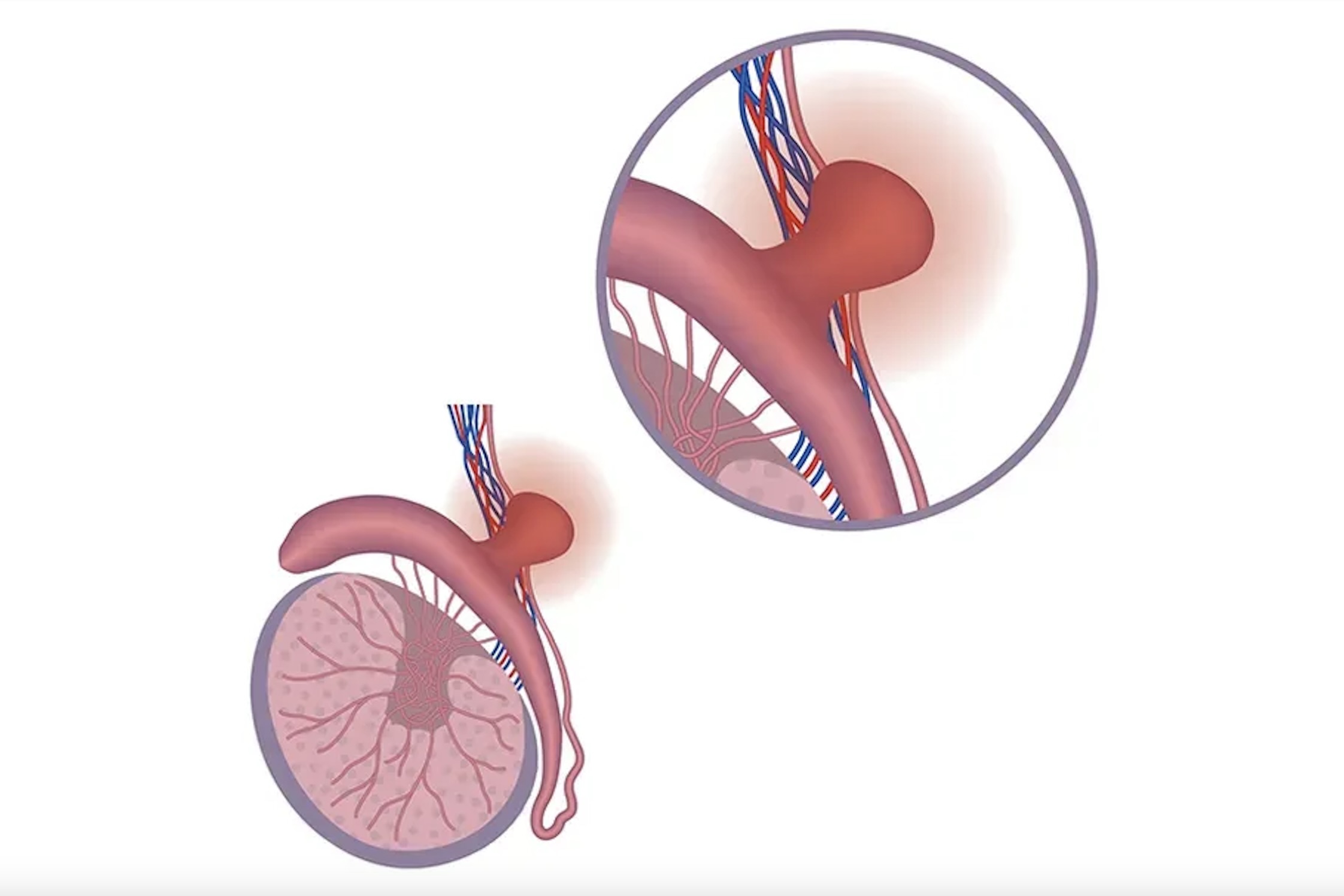
Spermatocele, also known as a spermatic cyst, is a benign (non-cancerous) fluid-filled cyst that forms in the epididymis, which is the coiled tube located behind the testicle that stores and transports sperm. Spermatoceles are usually painless and typically do not cause any symptoms. However, if a spermatocele becomes large or causes discomfort, it may cause the following symptoms:
- Palpable Lump: A small, smooth, and non-tender lump or swelling in the scrotum, usually located above or behind the testicle. The lump may be filled with fluid and feel like a small, firm sac.
- Heaviness or Discomfort: Some men may experience a feeling of heaviness or discomfort in the scrotum, especially if the spermatocele is large or if it is pressing on nearby structures.
- Enlargement of the Scrotum: In some cases, a large spermatocele may cause the scrotum to appear enlarged or swollen.
- Pain or Tenderness: Spermatoceles are typically painless, but if they become infected or inflamed, they may cause pain or tenderness in the scrotum.
- Changes in Size: Spermatoceles may change in size over time, becoming larger or smaller. They may also disappear on their own without treatment.
It’s important to note that spermatoceles are usually harmless and do not require treatment unless they cause significant discomfort or concern. If you experience any symptoms of a spermatocele or notice any changes in your scrotum, it’s important to see a healthcare provider for evaluation and appropriate management.
What are the causes of a spermatocele?
Spermatoceles are typically caused by blockages or obstructions in the epididymal ducts, which are the small tubes that transport sperm from the testicles to the vas deferens. These blockages can prevent the normal flow of sperm and fluid, leading to the formation of a cyst. The exact cause of these blockages is not always known, but they may be related to:
- Trauma: Trauma or injury to the scrotum or epididymis can cause scarring or damage to the ducts, leading to blockages and the formation of spermatoceles.
- Infection: Infections of the epididymis, such as epididymitis, can cause inflammation and scarring of the ducts, which may lead to blockages and the development of spermatoceles.
- Congenital Factors: Some men may be born with abnormalities or defects in the epididymal ducts that increase the risk of blockages and spermatocele formation.
- Obstruction: Obstructions in the epididymal ducts, such as from previous surgery or inflammation, can prevent the normal flow of sperm and fluid, leading to the formation of spermatoceles.
- Unknown Causes: In some cases, the exact cause of a spermatocele may not be known, and it may develop spontaneously without an obvious underlying cause.
It’s important to note that spermatoceles are benign and not typically associated with an increased risk of infertility or other serious health problems. However, if you have concerns about a spermatocele or notice any changes in your scrotum, it’s important to see a healthcare provider for evaluation and appropriate management.
What is the treatment for a spermatocele?
In many cases, spermatoceles do not require treatment, especially if they are small, asymptomatic, and not causing any problems. However, if a spermatocele is large, painful, or causing discomfort, or if it is affecting fertility, treatment options may be considered. Treatment options for spermatoceles may include:
- Observation: Small, asymptomatic spermatoceles may be monitored without intervention, especially if they are not causing any problems or discomfort.
- Pain Management: Over-the-counter pain medications, such as ibuprofen or acetaminophen, may help relieve pain or discomfort associated with a spermatocele.
- Aspiration: In some cases, a healthcare provider may use a needle to drain the fluid from a spermatocele, which can help reduce its size and relieve symptoms. However, this is not a permanent solution, and the spermatocele may recur.
- Surgery: Surgical removal of a spermatocele (spermatocelectomy) may be considered if the cyst is large, painful, or causing significant discomfort. During the procedure, the cyst is removed, and the epididymis is repaired. Surgery is usually done on an outpatient basis and is typically effective in relieving symptoms.
- Sclerotherapy: This is a less invasive procedure in which a sclerosing agent is injected into the spermatocele to shrink it. Sclerotherapy is typically used for smaller spermatoceles and may be less effective than surgery in larger cysts.
It’s important to consult with a healthcare provider for an accurate diagnosis and appropriate treatment recommendations if you have a spermatocele or if you have concerns about a scrotal lump. Treatment decisions will depend on the size, symptoms, and impact of the spermatocele on your quality of life.