Thyroid Cancer: Symptoms, Causes, Treatment
What are the symptoms of thyroid cancer?
Thyroid cancer often doesn’t cause any symptoms in its early stages. As the cancer grows, it may cause the following symptoms:
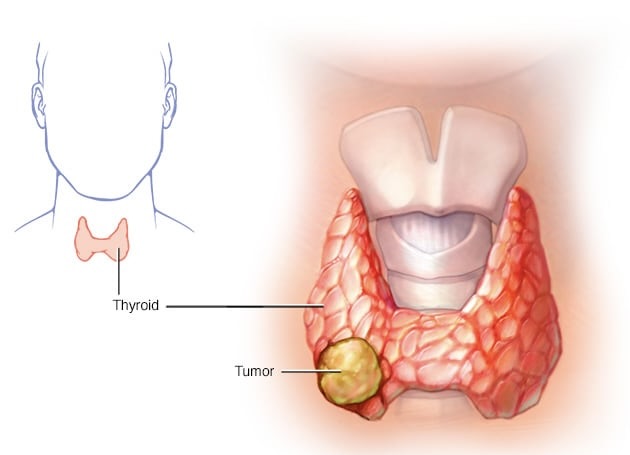
1. A lump in the neck: This is the most common symptom of thyroid cancer. It may be located in the front of the neck, near the Adam’s apple, or lower down where the thyroid gland is located.
2. Hoarseness or voice changes: Thyroid cancer can affect the vocal cords, leading to hoarseness or changes in the voice.
3. Difficulty swallowing: A large thyroid tumor can press on the esophagus, making it difficult or painful to swallow.
4. Neck or throat pain: Some people with thyroid cancer may experience pain or discomfort in the neck or throat, especially when swallowing.
5. Swollen lymph nodes: Thyroid cancer can cause swelling of the lymph nodes in the neck.
6. Breathing difficulties: A large thyroid tumor can compress the windpipe, leading to breathing difficulties, especially when lying flat.
7. Persistent cough: A cough that doesn’t go away or worsens over time can be a symptom of thyroid cancer.
8. Difficulty breathing or shortness of breath: This can occur if the cancer has spread to the lungs or if it is pressing on the windpipe.
It’s important to note that these symptoms can also be caused by other conditions, such as thyroid nodules or benign thyroid conditions. However, if you experience any of these symptoms, especially if they are persistent or worsening, it’s important to see a healthcare provider for a proper evaluation and diagnosis.
What are the causes of thyroid cancer?
The exact cause of thyroid cancer is not known, but several factors may increase the risk of developing the disease. These risk factors include:
- Gender: Thyroid cancer is more common in women than in men.
- Age: Thyroid cancer can occur at any age, but it is more common in people over the age of 30 and becomes more common as people get older.
- Radiation exposure: Exposure to high levels of radiation, such as radiation therapy for head and neck cancers or radiation fallout from nuclear accidents, increases the risk of thyroid cancer.
- Family history: Having a first-degree relative (parent, sibling, or child) with thyroid cancer increases the risk of developing the disease.
- Genetic conditions: Certain genetic conditions, such as familial medullary thyroid cancer (FMTC) and multiple endocrine neoplasia type 2 (MEN2), increase the risk of thyroid cancer.
- Thyroid nodules: People with thyroid nodules, especially those that are large or have certain characteristics on imaging studies, may have an increased risk of thyroid cancer.
- Iodine deficiency or excess: Iodine is essential for thyroid function, and both iodine deficiency and excess can increase the risk of thyroid cancer.
- Certain medical conditions: Some medical conditions, such as Hashimoto’s thyroiditis (an autoimmune thyroid disease) and goiter (enlarged thyroid), may increase the risk of thyroid cancer.
It’s important to note that having one or more risk factors does not mean that a person will develop thyroid cancer. Many people with thyroid cancer have no known risk factors, and many people with risk factors never develop the disease. If you have risk factors for thyroid cancer, it’s important to discuss them with your healthcare provider.
What is the treatment for thyroid cancer?
The treatment for thyroid cancer depends on the type and stage of the cancer, as well as the individual’s overall health and preferences. Treatment options may include:
- Surgery: The main treatment for thyroid cancer is usually surgery to remove all or part of the thyroid gland. The extent of the surgery depends on the size and location of the tumor.
- Radioactive iodine therapy: After surgery, radioactive iodine therapy may be used to destroy any remaining thyroid tissue or cancer cells. This treatment is often used for certain types of thyroid cancer, such as papillary and follicular thyroid cancer.
- Thyroid hormone therapy: Thyroid hormone replacement therapy is usually necessary after surgery to remove the thyroid gland. This medication helps to replace the hormones normally produced by the thyroid gland and helps prevent the growth of any remaining cancer cells.
- External beam radiation therapy: In some cases, external beam radiation therapy may be used to treat thyroid cancer, especially if the cancer has spread to nearby tissues or lymph nodes.
- Chemotherapy: Chemotherapy is not commonly used to treat thyroid cancer, but it may be used in certain cases, such as when the cancer is not responding to other treatments or has spread to other parts of the body.
- Targeted therapy: Targeted therapy is a type of treatment that targets specific molecules involved in cancer cell growth. It may be used in some cases of advanced thyroid cancer.
- Clinical trials: Participation in clinical trials may be an option for some people with thyroid cancer, especially those with advanced or hard-to-treat disease.
The specific treatment plan for thyroid cancer is individualized and may involve a combination of these treatments. It’s important for individuals with thyroid cancer to work closely with a healthcare team experienced in treating thyroid cancer to develop a treatment plan that is tailored to their specific needs.